I only had two pieces of BC-specific news, so I folded them in to the General post.
COVID-19
Pathology
IMPORTANT! This paper from USA (2024-06-21) reports using that cannabis raises your risk of severe COVID! The study found that people who used cannabis had a 28% higher risk hospitalization and 78% higher risk of ICU admittance than patients who had not used cannabis at least once in any form in the previous year. (NB: It’s not absolutely clear if it’s “smoking” or “using”. The paper says “smoking”, but in this article about the paper, one of the authors is quoted saying that they couldn’t tell if it was smoking, eating, vaping, or what.)
The study also can’t tell how often people used cannabis: the electronic records just record whether people used it “at least once” in the past year.
Still, if you use cannabis, you might want to consider increasing your mitigation efforts!
This paper from Canada (2024-06-21) reports that about half the people who had COVID-19 had signs of reduced oxygen in the brain. Using frequency-domain near-infrared spectroscopy (fdNIRS), they looked at cortical microvascular oxygenation, and found that 24% of people who had COVID-19 showed signs of hypoxia at least eight weeks after their infection.

This cerebral hypoxia correlated with nasty symptoms:

The patients were recruited from the general public, not from a Long COVID clinic or anything like that. However, 56% of the respondents said they had persistent symptoms, so maybe Long COVID patients preferentially enrolled in the study? Maybe it doesn’t matter: even if it were only Long COVID patients, it would still be an interesting result.
This paper from USA (2024-06-20) reports that babies born to mothers with higher pandemic stress had smaller brain volumes in a few places than babies born to less-stressed mothers.
Long COVID
This article from Simon Fraser (2024-06-21) gives a BC-centric view of the Long COVID experience.
This paper from USA (2024-05-24) reports that while there are a few Long COVID symptoms that women who get COVID-19 while pregnant are more likely to get than women who get COVID-19 when not pregnant, overall, women who get COVID-19 while pregnant are 15% less likely to get Long COVID. Compared to women who got COVID-19 while not pregnant, women who get COVID-19 while pregnant are
- 67% more likely to get an irregular heartbeat;
- 34% more likely to get abdominal pain;
- 88% more likely to get a thromboembolism;
- 65% less likely to get malaise;
- 64% less likely to get pharyngitis;
- 61% less likely to get cognitive symptoms.
This article (2024-06-07) reports that a brain fog clinic for military and police veterans has opened in Surrey. The article says its for brain fog from any source (e.g. concussions), but that 65% of the people who registered are Long COVID patients.
COVID-Related Excess Deaths and Sickness
This paper from USA (2024-04-05) found that people who had been infected with COVID-19 had more cardiovascular issues than those with non-COVID upper respiratory infections. Compared to people with non-COVID respiratory infections (influenza A or B, three of the common cold coronaviruses, human metapneumovirus, RSV, or rhinoviruses), people who had had COVID-19 infections had the following higher risks of abnormal readings on EKGs:
- 50% higher risk of an abnormal ischemic reading;
- 50% higher risk of an abnormal rhythm reading;
- 20% lower risk of an abnormal conduction delay reading.
This article (2024-06-18) reports on a Swedish study that found that the number of children who got Type 1 diabetes (T1D) rose by 62% from 2018 to 2022. Kids whose mothers had some COVID-19 immunity before they got pregnant — from either vaccination or infection — had lower rates of T1D.
Mitigation Measures
This paper from USA (2024-06-03) found (unsurprisingly!) that releasing COVID-19-positive patients to care homes was a really bad idea. Care homes which took COVID+ patients had 2.3 more fatalities per hundred residents compared to care homes which did not (a 31.3% increase over the mean). Care homes which took COVID+ patients and which also had shortages of PPE had 14.81 additional deaths per 100 residents compared to controls; care homes which took COVID+ residents that also had staff shortages had an excess 10.97 deaths per 100 residents.
This paper from Switzerland (2024-06-28) found that masking works. For an admittedly small sample size, they found that hospitals which switched from policy of less masking to more masking saw a 61% reduction in hospital-acquired COVID-19 infections.
If you are trying to do COVID-safe things, the Victoria Bug Museum has a safe time every day they are open: the first two hours requires masks for everyone over five.
I wish that there were safe hours or safe days for all kinds of things. What if masking was required in all health care settings all day on Mondays, for example?
This article (2024-06-27) reports that 91% of Public Service Alliance of Canada union members are against return-to-office mandates. (All federal public servants are supposed to be in the office at least three days per week, starting on 9 Sep 2024.)
Vaccines
This press release reporting on a conference presentation (2024-06-11) says that vaccinated adults who already had heart failure had 82% lower risk of all-cause mortality, 47% lower risk of hospitalization for heart failure, and 13% reduced risk of COVID-19 infection compared to unvaccinated people who had previous heart failure.
This paper from Singapore (2024-06-26) reports that people who got an XBB 1.5 booster or bivalent booster did better against JN.1 infection than people who did not.
Compared to people who only got a monovalent COVID Classic boosters or an old infection, people who got more recent boosters had lower risks of various unpleasant outcomes:
| Outcome | Booster | Relative Risk |
| infection | XBB 1.5 | -41% |
| infection | Classic/BA.5 | – 8% |
| ED visit | XBB 1.5 | -50% |
| ED visit | Classic/BA.5 | -20% |
| ED visit | infection <120 days prior | -35% |
| hospitalization | XBB 1.5 | -48% |
| hospitalization | Classic/BA.5 | – 0% |
This paper from USA (2024-06-24) also reports that the vaccine effectiveness of the Pfizer XBB 1.5 booster is good. Relative to people who did not get an XBB 1.5 booster, the vaccine effectiveness of the Pfizer XBB 1.5 booster (at a median of 34 days before) was 58% against ED visits and 62% against hospitalization. They also found that people who had older vaccinations were no better off than people who had never been vaccinated. Vaccine effectiveness wears off, y’all!
This paper from USA (2024-06-18) says that women report more local adverse effects (AEs, AKA side effects) from COVID-19 or flu vaccines than men do. (Local AEs are side effects specifically at the injection site — like swelling or pain at the injection site.) Interestingly, men and women had similar systemic AEs (things like fatigue or nausea). I wonder if partly it’s because men are trained not to report pain? Or maybe it’s because the vax doses are the same regardless of body mass, and men have (on average) higher body mass than women.
The study also found that more women than men scheduled their shots for the day before days off so that they would not miss work.
This paper from USA (2024-05-31) reports that misinformation on Facebook which was true but misleading led to 46 times as much vaccine hesitancy than out-and-out false (and tagged as false) posts.
Variants
This preprint (2024-06-09) says that LB.1 has an even higher R(effective) than KP.2 or KP.3. Note that LB.1 is not a descendent of KP.2 or KP.3, it’s more like a cousin — LB.1 is formally JN.1.9.2.1, vs. JN.1.11.1.2 and JN.1.11.1.3. Thus maybe it’s okay to get a JN.1-based vaccine (i.e. Novavax) instead of a KP.2-based vaccine (i.e. Pfizer or Moderna).
Testing
This paper (2024-06-24) reports that you can tell if someone has COVID-19 from their breath with high accuracy. They collected breath from PCR-positive people with either Alpha or Delta variants with microfabricated silicon microreactor and analyzed it with ultra-high-performance liquid chromatography-mass spectrometry. This sounds great, but I don’t know how expensive this equipment is.
Treatments
This paper from USA (2024-06-26) reports that Remdesivir worked very well on hospitalized COVID-19 patients. Patients who got Remdesivir were 54% less likely to die, and 64% more likely to be discharged within 28 days than those who did not get Remdesivir.
Recommended Reading
If you want a quick reminder of why you don’t want to catch COVID-19, or need to tell the people who keep hassling you why you don’t want to catch COVID-19 (or why they shouldn’t keep catching COVID-19), this (2024-05-31) and this (2024-06-13) are excellent summaries.
BC
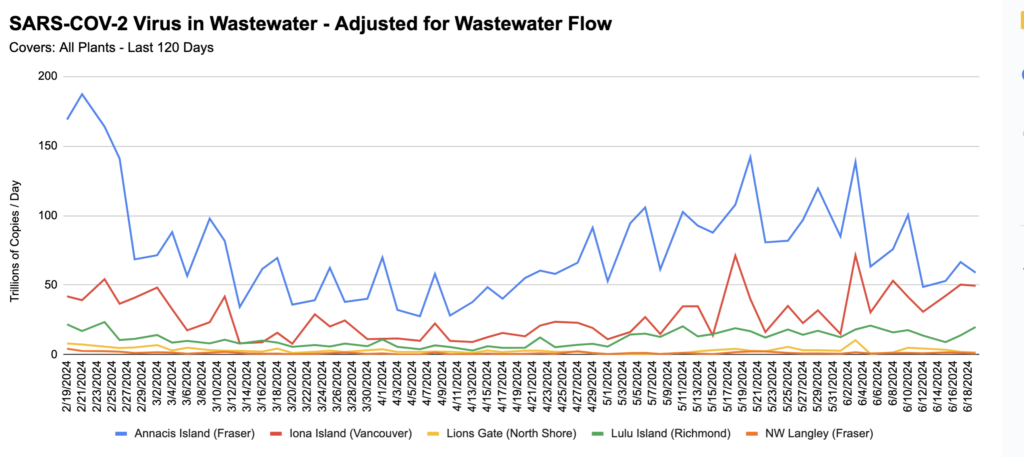
From Jeff’s wastewater spreadsheet:
HPAI (Highly Pathogenic Avian Influenza)
Transmission
This USA FDA report (2024-06-28) found that pasteurization (using commercial pasteurization equipment) killed all the H5N1 in artificially-infected milk.
Note that this was not milk from an infected cow: they took raw cow milk and put high levels of H5N1 isolated from a turkey into the milk. This is a much closer match to reality than the study I reported on last time, which used lab equipment to pasteurize milk infected with H5N1 isolated from a mountain lion. However, it’s still not a commercial pasteurization process with milk from an infected cow.
This article (2024-06-27) reports that there are now 132 dairy cow herds in 12 US states with H5N1 infections. (I still have not heard of any herds outside of the US which have infections.)
This preprint (2024-06-24) reports that H5N1 and human H1N1 both stay infectious on milking machine equipment for several hours. (This is not a surprise.)
Recommended Reading
This article (2024-06-20) talks about how the USA is being really slow to test for H5N1 and why.
