COVID-19
Long COVID
🙁🛌 This preprint using data from USA and UK (2025-03-01) reports that people with hypermobility are at increased risk of Long COVID. People with generalized joint hypermobility have a 29% higher risk of Long COVID than controls; people with extreme hypermobility have a 112% higher risk than controls. This higher risk is both from:
- a higher risk of harsher symptoms in the acute phase of COVID-19, which is itself a risk factor, and
- higher risk of Long COVID than non-hypermobile people who have the same symptom severity in the acute phase.
🗡️🩸 This paper from UK (2025-03-01) reports that people who eventually developed Long COVID had more problems with iron than people who got COVID-19 but not Long COVID. People who got Long COVID had blood signatures which included a word salad of things mostly related to iron dysfunction, including: anemia, low serum iron, altered iron-homeostasis gene expression and stress-production of red blood cells. (No, I don’t understand what all of those all, but they all have to do with blood.) The severity of the acute infection didn’t make an independent difference, what mattered was the iron dysfunction.
🛌 This paper from UK (2025-03-05) reported on risk factors for developing Long COVID:
- each additional year of age increased the risk of Long COVID by 6.4% ‼️;
- Asian or Asian-British people had a 164% higher risk of Long COVID;
- former smokers had a 544% ‼️🤯 higher risk;
- people who had interstitial lung diseases had 193% higher risk;
- people who had high Clauss figbinogen levels had a 22% higher risk.
📚🛌 This paper from Australia (2025-03-05) found that cognitive deficits following COVID-19 were 33 % smaller among people with high “cognitive reserve (CR)” individuals, and 33 % greater among low CR individuals, relative to those with average CR. (Cognitive reserve is estimated with more education and cognitively complex occupations giving higher CRs.)
🛌 Orexins are peptides which regulate some of the most primal bodily functions, including arousal, wakefulness😳, and appetite 😋. That sounds to me like autonomous nervous system stuff, which seems like what gets messed up in bad Long COVID. This review paper (2025-02-21) suggests that Long COVID is caused by disrupted a orexin system.
When looking up orexins, I found this paper from USA (2002-05-25) reports that fasting raises the levels of orexins.
That made me go waitaminute, because I had this video about fasting cued up that I hadn’t watched yet. I watched it. In it, a guy (Gez Medinger) talks about extended fasting as Long COVID treatment. He says that he’s a long hauler, and that supervised extended fasting — several weeks, with a little bit of broth and a little bit of fruit juice under medical supervision — helped him.
So maybe fasting Long COVID is caused by low orexin levels, fasting causes increased orexin levels, which makes the Long COVID better. Maybe?
Medinger also likens extended fasting as being like “rebooting the human”. Meanwhile, I have been amazed that a stellate ganglion block frequently gives people their sense of smell back, and I think of the stellate ganglion block as “rebooting the autonomic nervous system”.
Now, Medinger might be a charlatan, I am not a doctor, not an expert, this could all be coincidences, but I thought it was interesting. I was especially struck that orexin/Long COVID, orexin/fasting, and fasting/Long COVID came at me simultaneously from two different directions!
NB: It is very important to not try eating-almost-nothing-for-several-weeks at home!
👃👅 Because I was curious about the fasting thing (above), I dug into stellate ganglion blocks’ effects on Long COVID (not just on smell/taste disturbances). This cases study paper (2024-06-12) found that ten people out of 27 had significant improvements after a stellate ganglion block:
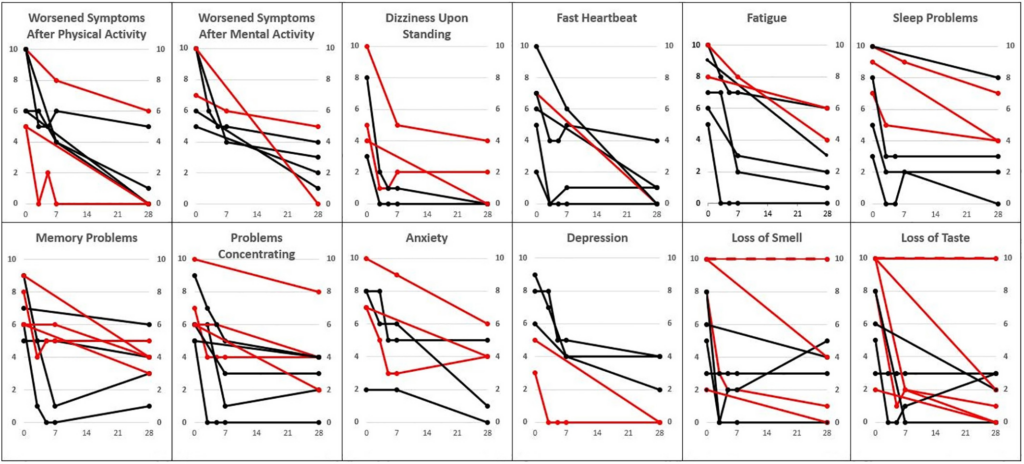
Ten people responded really well to treatment and two didn’t respond at all; the other fifteen partially responded, and got a second treatment — which meant that their data couldn’t honestly be used in this comparison. NB: The two who did not respond at all to treatment were two of the three people who only had smell/taste issues, for what that is worth.
👃🔪Okay, this is strange. This paper reports from Italy (2025-02-24) reports that people who lost their sense of smell from a COVID-19 infection got a significant improvement in their ability to smell after functional septorhinoplasty (fSRP) — surgery to repair a deviated septum. All of the people who had the surgery had deviated septums, and all had improved airflow after the surgery, which other papers (including pre-pandemic papers) say improves sense of smell. So it might not have anything to do with COVID-19, it might have to do with blocked noses. However, these surgeries are done under general anesthetic and operate near the olfactory bulb. Maaaaaayyyybe the anesthetic, or cutting near the nose rebooted the autonomic nervous system?
COVID-Related Excess Death and Sickness
🧠 😢This older paper from USA (2023-05-02) reports that high school athletes who had had COVID-19 infections had three times the risk of concussions as those who had not had COVID-19 infections.
This paper from UK (2024-08-12) found that 14% of participants had adrenal insufficiency during their acute COVID-19 phase, and 13% had adrenal insufficiency at one year — although all the patients got better by the second year.
🛌 This paper from Japan (2025-02-19) reports that they have found two biomarkers for Long COVID: autoantibodies targeting PITX2 (known to be involved in cardiac function and nerve development) and FBXO2 (known to be involved in various regulatory functions and theorized to be involved with neurodegenerative conditions). Not only that, but FBXO2 autoantibody levels were associated with shortness of breath and loss of appetite, while PITX2 autoantibody levels were associated with fever, heart palpitations, loss of appetite, and brain fog
(PITX2 is known to be involved in cardiac function and nerve development; FBXO2 is known to be involved in various regulatory functions and FBXO2 autoantibodies are theorized to be involved with neurodegenerative conditions).
Pathology
🏥☠️ This paper from Hong Kong (2025-01-19) found that patients hospitalized for the second time for COVID-19 were 37% more likely to die than patients who were hospitalized for the first time for COVID-19. It’s almost like damage is cumulative.
🏭☠️ This paper using data from UK(2025-03-03) reports that air pollution and genetics both raise the risk of severe COVID-19 outcomes.
For each interquartile range–rise in air-pollution concentrations, the risks of COVID-19 infection were 96% higher for PM2.5 and PM10, 97% for NO2, and 98% for NOx.
People who had both high genetic risk and high exposure to pollutants were ~90% more likely to be hospitalized and ~twice as likely to die as those with low genetic risk and low pollution exposure.
🤔 This paper from China (2025-03-01) found that the levels of trace metals were different in recovered COVID-19 patients from levels in people who hadn’t had COVID-19 infections.
- Levels of Cu, Ag, As, Ba, Cd, Ni, Pb, Cr and V were higher.
- Levels of Fe and Se were lower.
- Levels of Zn, Mn, and Co were about the same.
Testing
🇺🇸 Apparently, anybody in the USA can order a huge amount of rapid tests from the government (minimum order of 300!) by following the steps in this form.
Mitigation Measures
😷 Do you still mask? Do you have people tell you that your masking is a sign of mental illness? Then send them this takedown (2025-01-25).
Vaccines
👍💉This paper (2025-03-05) reports on a viral-vector vaccine with both SARS-CoV-2 and influenza spikes* which gave long-lasting protection in mice. The vaccine uses a version of the vesicular stomatitis virus (VSV) (but don’t worry, they neutered it first so it can’t replicate).
The vaccine uses slightly different spikes than other vaccines. For the SARS-CoV-2 spikes, they removed the furin cleavage site (which I believe means that the spike stays locked in the position they are normally in when they are floating around and not actively trying to muscle into a cell). For influenza, they use the neuraminidase protein (the “N” part of H5N1) instead of the hemagglutinin protein (the “H” part of H5N1), while the majority of flu vaccines use the H protein. N is more conserved than H, meaning it doesn’t change as fast as H.
It is not clear to me how much of the vaccine’s success against COVID-19 is due to having the immune system train against flu at the same time, how much is due to not having a furin cleavage site, and how much is using that specific viral vector. I don’t know how much the influenza protection is from using the N part, how much is having a SARS-CoV-2 part, and how much is from using that specific viral vector.
*They don’t actually use the term “spikes” for the pointy-outy bits on influenza viruses which unlock host cells, analogous to the spike proteins on SARS-CoV-2, but it was convenient for me to use the term.
💩💉 That preprint on vaccine injuries (2025-02-25) I mentioned in last week’s General post which generated a shitshow? Here’s a detailed critique (2025-02-24) if you happen to be arguing with someone about it.
Treatments
(See above in the Long COVID section for some papers which include treatments for Long COVID, including stellate ganglion blocks, extreme fasting, and and nose surgery.)
💊 This paper from Hong Kong (2025-02-28) reports that Paxlovid is better for asthmatics than molnupiravir. Asthmatics who got Paxlovid for COVID-19 infections were 35% less likely to be hospitalized than ones who got molnupiravir. Paxlovid also helped with treatment issues: asthmatic patients who were given corticosteroids plus Paxlovid had a 48% lower risk of asthma exacerbation than those who got corticosteroids plus molnupiravir.
💊 This paper (2025-03-07) reports that Long COVID decreases the levels of peroxisomes in macrophages (a type of white blood cell). (Peroxisomes are biological mini-machines which, among other things, chops up long-chain fatty acids into the medium-chain that mitochondria then eat.) The authors demonstrated that peroxisomes in macrophages were essential for reducing inflammation and repairing lung tissue damage.
🎉 The best news? Sodium 4-phenylbutyrate (4-PBA) was known to increase peroxisomes (from this paper (2005-02-24)), and the 2025-03-07 research verified that 4-PBA helped mice recover better from COVID-19 lung damage!
4-PBA isn’t exactly a drug, it’s a prodrug — it’s a chemical which the body turns into a drug. I am guessing that means it is cheap and unencumbered by patents.
Novel Coronavirus
Discovery
🤯This paper from South Korea (2025-02-21) reports that a novel coronavirus was discovered in a baby two years ago. This coronavirus is an alphacoronavirus (COVID-19 is a betacoronavirus), and is related to a rodent-derived virus (AcCoV-JC34). Before you freak out, I’d like to remind you that there are four other coronaviruses which commonly circulate in humans as “common colds” (plus in 2018 they found a dog coronavirus in people and then that same strain in Haiti in 2021). Also, if it was that bad, it would have spread more in the past two years.
H5N1
Transmission
🐖🐦⬛This paper (2025-03-05) reports that pigs can be infected with H5N1, but don’t appear to transmit it 🎉. Laboratory pigs were deliberately infected with cow-type bird flu🐄🐦⬛, but pigs who were housed with the infected pigs did not get sick themselves.
The paper also mentions that pigs aren’t as susceptible to the H5N1 strain that comes from cows🐄🐦⬛ (clade B3.13) as they were to the H5N1 strain that comes from minks or to non-H5N1 pig-adapted influenza.
🐄🐦⬛This article (2025-03-04) reports that there have been 977 H5N1 outbreaks in dairy cattle from 17 states.
🐈⬛☠️🐓🐦⬛The article also reports five more housecat deaths in Washington and Oregon, which might be related to the Wild Coast raw pet food. However, there was also one housecat death in New Jersey and one in Colorado, and Wild Coast doesn’t sell in those jurisdictions.
Mystery Illness
☠️ This article (2025-03-04) reports that the World Health Organization now thinks that the mystery illness in DR Congo is likely to be chemical poisoning or rapid-onset bacterial meningitis.
Mpox
🎉💉 This article (2025-03-06) reports that mpox cases in DR Congo — especially in health care workers — are falling. One thing they’ve done to contain it: 300,000 people have been vaccinated in Kinshasa (the capital) in the past ten days.
☠️☠️ Unfortunately, there has been fighting in one of the areas with the worst outbreak. The article says that 605 mpox patients had to flee health centers because of fighting, and only about 150 have made their way back.
