H5N1
Transmission
This article (2024-11-12) reports that a teenager from BC in the Fraser Health Authority region is in critical care with the bird-version of H5N1 (clade 2.3.4.4b, genotype D1.1, i.e. not the cattle version). Nobody knows how the teen caught it — the teen had contact with other people, dogs, cats, and reptiles, but pretty serious contact tracing hasn’t turned up any other living being they could have caught it from. Furthermore, the more time passes, the more memories get weak, and the less likely they will find a link; pub health is now saying that they probably will never know.
I don’t think this is nefarious or shady. There are a lot of birds in BC, and they breathe in and out all the time. I suspect that the teen was near enough to an infected flock that they inhaled some bird flu and got sick. (I’m imagining, for example, the neighbourhood in Burnaby where all the Metro Van crows go at night. What if the teen’s bedroom is on the second floor overlooking that flock of crows? (Yes, I know a flock of crows is called a murder. With the teen’s life on the line, I don’t think that’s funny right now, so don’t make that joke to me.)) This is disturbing, this should be disturbing, because it means that you and I are also at risk from random birds. Sorry.
I find it a little concerning that the teen got so sick.
- The article says that the teen did not have any underlying health issues.
- Young people are supposed to have strong immune systems! (Although, this article (2024-11-12) notes that young people might not have been exposed to H1N1 before, possibly giving them less protection than older people whose immune systems have bumped into the N1 type-1 neuraminidase before.)
- Every other person who has gotten sick from cattle-H5N1 or poultry-H5N1 in the US had a mild case. (Possible exception: the Missouri case, which also was the only other unknown-transmission-chain case in North America. The Missouri person had a lot of underlying health issues, and I believe the H5N1 was noticed when they went into the hospital for those other health issues.)
Interestingly, the teen had an eye infection (as well as a cough and fever). Many of the people with cattle-H5N1 had eye infections as well.
This article (2024-11-15) says that the US has identified 508 infected dairy herds and poultry flocks in 15 states, with 291 of them in California.
Vaccines
This article (2024-11-13) says that Health Canada has authorized three different vaccines for use against bird flu. (Interestingly, I couldn’t find out any information on the Public Health Canada website (or anywhere) about those three vaccines, but the article says GSK makes one locally and can accelerate if needed.) The article says that the government has no stockpile because the vax only has a shelf life of two years, which honestly? seems sort of reasonable to me:
- Human-to-human spread appears to be very rare.
- Cases are usually mild. Yes, there is a teen in intensive care, but that’s the only severe case we’ve seen in North America. Yes, it is hugely deadly in birds, but humans aren’t birds.
- There are a number of really promising universal-influenza vaccines in the pipeline. (See here (2022-11-02), here (2024-01-16), here (2024-09-16), here (2024-03-21), Phase 2b trial start here (2023-11-27), Phase 1 trial start here (2024-09-15).) This influenza virus tracker shows that there are 255 vaccines in the pipeline, and some of them are universal vaccines. I counted at least five Phase 2 trials of universal vaccines.)
- We humans have proven that we can make vaccines really fast in a crisis.
- We have learned a lot about coping with airborne diseases. Improving ventilation decreases risk. Masking with N95 really decreases risk. Nasal irrigation significantly decreases risk. Working remotely decreases risk. We can do this if we have to.
I am NOT saying “there is nothing to worry about”, but I think there are more productive things to worry about RIGHT NOW. (I will tell you when you need to freak out, don’t worry.)
COVID-19
Long COVID
⭐ This paper from Hungary (2024-11-04) reports that mitochondria are F’d up in people with Long COVID. They found microstructural abnormalities in mitochondria via transmission electron microscopy, and they found elevated levels of cell-free mitochondrial DNA circulating in blood — which could be used as a Long COVID marker.
AGAIN This paper from USA (2024-11-13) reports that adults who got three mRNA doses had lower risks of Long COVID symptoms than unvaccinated controls:
- 63% lower risk of gastrointestinal symptoms;
- 44% lower risk of neurological symptoms;
- 52% lower odds of other symptoms.
Pathology
This paper from Switzerland (2024-11-13) reports that hospitalized patients with COVID-19 had very similar outcomes to patients with influenza. They went into the ICU at about the same rate, and died at about the same rate. However, there were about 50% more COVID-19 patients per month than influenza patients per month during the study period.
This paper from China (2024-11-12) reports that a genetic predisposition to gastroesophageal reflux disease (GERD), raises the risk of hospitalization for COVID-19 by 33% and the risk of severe COVID-19 by 27%. (Unfortunately, I couldn’t figure out what their definition of “severe” was. Most papers equate “severe” with “hospitalized”, but clearly that’s not happening here.)
COVID-Related Excess Death and Sickness
⭐ This paper from Italy (2024-09-12) reports getting COVID-19 increases the risk of dyslipidemia (abnormal cholesterol or lipids) by 29%. For this study, dyslipidemia meant having high total cholesterol, low HDL (“good cholesterol”), high triglycerides, or prescriptions for lipid-lowering therapy. (Abnormally low cholesterol apparently wasn’t interesting — or doesn’t happen.)
Treatments
This paper from Austria (2024-11-03) reports that Paxlovid is very useful in adults over 60, but not in adults under 60. They found that for adults over 60, Paxlovid reduced the risk of hospitalization by about half; 0.13% of the non-Paxlovid patients died and none of the Paxlovid patients died.
They also found that molnupiravir didn’t help (and maybe — if I read it right — was harmful).
AGAIN This paper written by Pfizer researchers in the USA (2024-11-11) reports that Paxlovid works really well in high-risk, unvaccinated, nonhospitalized (when they started the study), symptomatic adults. Patients who ended up hospitalized despite the Paxlovid had shorter stays than the hospitalized placebo group; none of the Paxlovid group required ICU admission or mechanical ventilation, and none died. Non-hospitalized people got over COVID-19 on average in 13 days instead of 15.
Pathology
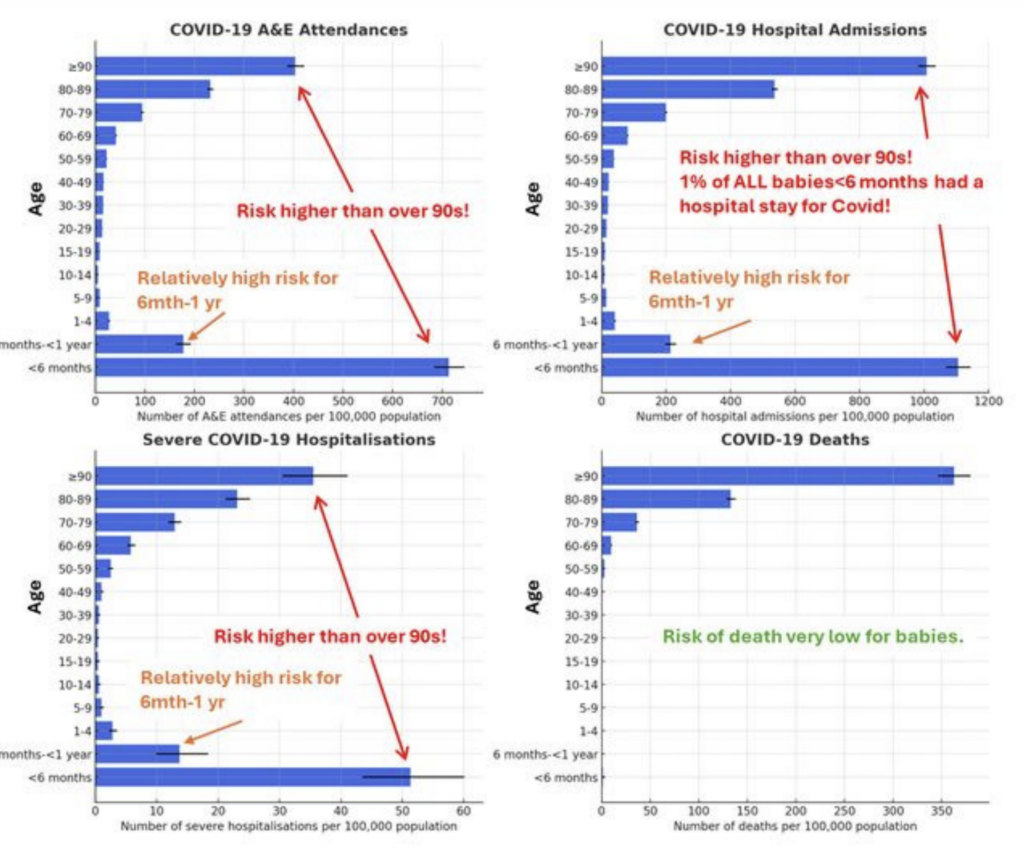
⭐ This preprint from UK (2024-11-11) found that children under six months old are hugely susceptible to severe COVID-19 (although they don’t usually die from it.) Here’s a graph using the preprint’s data that someone else made in this blog post (2024-11-13):
I have also seen several people on teh socials posting about this. Here’s two graphs from this thread, for example, about hospitalization of children in Alberta.


This is consistent with this paper (2024-10-17) I posted about two weeks ago which found that babies under a year old accounted for 64% of pediatric hospital admissions in the UK, and this preprint (2024-11-13) which found that babies had high rates of emergency department admissions and hospitalization.
Presumably the babies are susceptible because they haven’t seen COVID-19 before. (Pregnant mothers! Get a vaccination, as that will give your baby some protections!)
Vaccines
AGAIN This paper from Italy (2024-11-14) reports that unvaccinated people do a lot worse than vaccinated people when hospitalized for COVID-19.
- 18x more likely to need low-flow nasal oxygen therapy;
- 4.65x more likely to need high-flow nasal oxygen therapy;
- 5.65x more likely to go to ICU;
- 5.83x more likely to get intubated;
- at two months, 20.3x more likely to have ground-glass opacities;
- 5.33x more likely to have myocarditis;
- infinitely more likely to have a pulmonary embolism;
- at one year, 20.5x more likely to have shortness of breath;
- at one year, 2.85x more likely to have psychological symptoms;
- at one year, 2.54x more likely to have chronic rhinosinusitis/cough.

1 comment
Comments are closed.