Vaccines
This paper from Italy reports on Novavax Classic effectiveness during the early Omicron period. In people who had no vaccination previously, after about two weeks post-dose, they found vaccine effectiveness to be:
| Against | infection | symptomatic infection |
| 1 dose | 23% | 31% |
| 2 doses | 31% | 50% |
You might look at this and think, “wow, that’s pretty crappy”, but remember two things:
- The vaccine used a COVID Classic spike during a time of Omicron.
- Unlike the controls during the initial Pfizer and Moderna trials, some of the controls here would have had prior infection.
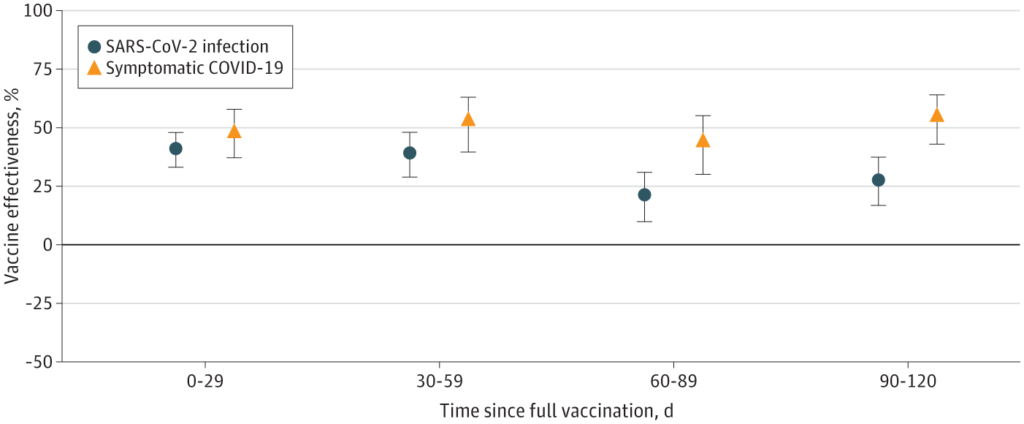
The estimated vaccine effectiveness did wane over time:
Again, you might think that’s pretty crappy, but other vaxes wane really fast also, sometimes faster. This paper from Denmark found really astonishingly crappy effectiveness against Omicron (green) after just three months:

From this paper from Qatar:

(Why is effectiveness negative after seven months? I’m not sure, but I suspect that the controls had infections more recently than the vaccinees had vaccines.)
This paper from USA describes vaccinating mice with a modified form of the MMR vaccine that gave broad and durable protection. They inserted three different spike proteins (from COVID Classic, Delta, and Omicron BA.1) with the 6-proline modification into three different viruses (one measles, two different mumps) and then gave it to mice. They did a mix of subcutaneous and intranasal, and found that intranasal-only was just as good as mixed. They found that the antibody levels induced by the trivalent vax were high and stayed high for at least four months. When they infected the mice with Classic, Delta, or BA.1, the mice were fine, losing very little weight if any
This article has an interview with a scientist who has been very knowledgeable and trustworthy throughout the pandemic, and he says some things which discourage me.
- While he thinks that COVID-19 will just be like any other cold for today’s babies — they will catch it over and over again and develop long-term immunity from it. he thinks that today’s elderly will never get robust immunity. They just won’t have enough time left in their lives to get exposed enough times, especially given how their immune systems just aren’t very good.
- Vaccines which we used to think gave sterilizing immunity (like chicken pox or measles) actually don’t. He said that it used to be that nobody got shingles until their 70s, but now we’re seeing it in people in their 30s. He said that’s because it used to be that you’d encounter chicken pox many times throughout your life, and every time you saw it (after your first infection or inoculation), your immune system would get reminded that the disease existed and it should pay attention to it. It was like a natural booster.
- Diseases like chickenpox and measles have to get deep into the body before they can start replicating, which means that your body has quite a while to mount a defence, which means it’s generally so successful that we don’t even notice the attack. With upper respiratory infections like COVID-19, they can start replicating pretty much immediately, so your body just doesn’t have time to mount an immune response.
- Long COVID isn’t strange, viruses are just nasty. We’ve always had Long X, we just didn’t have SO MANY PEOPLE get the same virus at once, so we couldn’t draw a line as easily between virus and Long X. And viruses are nastier when you have zero immunity to them.
In other words, there will never be a long-lasting vaccine that completely prevents COVID-19. 🙁
The one encouraging thing he did say was that the number of Long COVID cases per COVID-19 case is going down.
As this article describes, one way of modelling growth rates of contagious diseases is with DOTS: duration, opportunity, transmission probability and susceptibility. There was a different article that I can’t find now which talks about how, if a disease has been around a long time, it’ll be kind of in equilibrium with the disease because the opportunity and susceptibility will balance with the immunity the population has built up. But if the transmissibility is even a little higher in one season, then it could break out and lead to a wave of cases. This, my mystery author said, explains flu being seasonal. However, with a new disease like COVID-19, the improved transmissibility gets swamped by the susceptibility to new variants.
This paper (2023-08-31) from Australia looked at the relative benefits of Pfizer, Moderna, AZ, and Novavax. Pfizer was the best. Compared to Pfizer, the increased risk of getting COVID-19 with one of the other shots was:
| as primary series | as booster | |
| Moderna | +3% | +2% |
| AZ | +19% | +20% |
| Novavax | +70% | +39% |
As I’m a Novavax stan, this was hard for me to read.
This preprint from USA found that for mRNA vaccinations, the worse the post-vax side effects, the better the immune system response was.
This paper from USA from 2021 also found that the more side effects, the more antibodies, however, they also found that 98% of the people with no symptoms did develop antibodies.
The big UK mix&match study finally came out (in August, but I uh missed it). There’s a lot of little details in the study, I’m not going to try to summarize it all, but the big tl;drs are that mixing vs. matching doesn’t really seem to get you anything significant, that the mRNAs are really good, and AZ is not as good. Novavax is in the middle.

This case study from Japan found one man had leg pain after his first dose of Pfizer, followed by Deep Vein Thrombosis and a pulmonary embolism after his second dose.
Long COVID
This paper from UK says that people with acute respiratory infections also sometimes get symptoms that last at least four weeks. “Long Colds”.

This case study from USA said that three middle-aged people with Long COVID had a complete remission after a course of casirivimab/imdevimab monoclonal antibodies.
This paper from UK found that people who had been hospitalized with COVID-19 later had more organ abnormalities than controls. However, the controls had not been hospitalized; I would have preferred if they had compared people who had been hospitalized with COVID-19 versus those hospitalized for influenza or pneumonia. :-/
This article says that ACT scores in the US dropped with the school disruptions — and keep dropping.

I saw someone on Mastodon (sorry, can’t remember who, sorry) wonder if scores were still dropping (even though school closures were over) because of COVID-induced cognitive impairment. While that’s possible, I suspect it’s more likely that we still haven’t graduated kids whose education was impacted by pandemic upheavals or lots of teachers died or quit.
COVID-Related Excess Death and Sickness
This paper from Korea yet again found that rates of various conditions were higher after COVID-19 than before:
- 12% higher risk of alopecia areata (spot baldness);
- 74% higher risk of alopecia totalis (losing all the hair on the head and face);
- 176% higher chance of antineutrophil cytoplasmic antibody-associated vasculitis;
- 68% higher chance of Crohn’s disease;
- 59% higher chance of sarcoidosis.
This paper from Canada found that people with immune-mediated inflammatory diseases (IMID) were 21% more likely to get a venous thromboembolism after getting COVID-19 than those without an IMID.
Transmission
This paper from March 2021 from USA found that in a cohort of health care workers 1-hour longer sleep duration at night was associated with 12% lower odds of COVID-19. Also, reporting burnout ‘every day’ was associated with 160% greater risk of getting COVID-19! So chill and get some sleep.
Pathology
This paper from USA found that 1.5% of patients hospitalized with COVID-19 had sepsis from COVID (as opposed to picking up bacterial sepsis in the hospital).
This paper from Ontario found that care home residents who had been infected with BA.1 or 2 infections had a higher risk of then getting a BA.5 infection than people who had not gotten a BA.1/2 infection. All of the residents had had four monovalent mRNA doses!

This preprint from USA also found that prior infections were not protective after Omicron, and that people who caught it once were 64% more likely to catch it again. This might just mean that people whose lifestyle made them more likely to catch Omicron were likely to keep doing risky things, and thus catch it again.
However, note that the first study found that people who had a pre-Omicron infection weren’t particularly likely to get BA.5, and you would think people who caught COVID-19 pre-Omicron were more risk-tolerant than those who only caught it in Omicron.
This paper from Hong Kong found that there were significant changes in the signature of bacteria in breast milk after vaccination (with Pfizer), but that the changes were benign.
This article from USA found that cannabis users had significantly lower health complications from COVID-19 when hospitalized. The effect was not small: l
- 6.8% were intubated vs 12% of controls;
- 2.1% had acute respiratory distress syndrome (ARDS) vs 6% of controls;
- 25% had acute respiratory failure vs 52.9% for controls;
- 5.8% had severe sepsis with multiorgan failure vs 12% of controls;
- 1.2% had in-hospital cardiac arrest vs 2.7% of controls;
- 2.9% died vs 13.5% of controls.
Note that it wasn’t clear if this was only people who smoked weed or if this also applied to people who chowed on edibles.
This article from USA from August 2022 had similar findings, also among hospitalized COVID-19 patients:
- 5.1 NIH severity score vs. 6.0 for controls;
- 4 days of hospitalization vs. 6 for controls;
- 12% admitted to ICU vs. 31% for controls;
- 6% needing mechanical ventilation vs. 17% for controls.
Both papers mentioned immunomodulatory properties of cannabis. The second paper said that cannabis users had lower measured levels of various inflammatory markers.
However, this paper from UK from April 2022 found that cannabis users users were only 80% as likely to catch COVID-19, but were 2.81 times as likely to die.
(One difference between the first two papers and the third was that the first two only looked at people who had been hospitalized with COVID-19, while the third looked at a group of patients with evidence of COVID-19 infections in their blood.)
This paper from Australia found that children with asthma were not at higher risk from COVID-19 than non-asthmatic children.
Recommended Watching
This article talks about how Long COVID (and actually, COVID-19, period) in kids is under-diagnosed.
