Long COVID
This paper from USA is yet another which says that people are more likely to develop diabetes after a COVID-19 infection than the uninfected. In this paper, they found an adjusted increased risk of 58%.
This study from NY found that racialized COVID-19 patients did worse than white ones. (NB: This is not entirely surprising, given how pulse oximeters overestimate the concentration of oxygen in the blood of dark-skinned people.) Of people testing positive in the study, about 27% of Black COVID-19 patients were hospitalized, 25% of Hispanics were hospitalized, but only about 15% of Whites were hospitalized.
The symptoms the Whites/Non-Whites had had some big differences. For example, compared to hospitalized Whites, Blacks who were hospitalized were almost twice as likely to get diagnosed with diabetes, and ~50% more likely to get diagnosed with headaches. Compared to hospitalized Whites, Hispanics were about 60% more likely to have headaches and ~20% more likely to have shortness of breath.

This press release from the US NIH talks about one study from NY (see above) which says that poor racialized minorities have more Long COVID and another study which says that women from more high-income areas had more Long COVID. They pointed out that women are more likely to seek care, which means that there might be a bunch of Long COVID cases which aren’t getting diagnosed. (It might also clear that Long COVID patients get gaslit lot; women probably have more experience dealing with gaslighting; wealthy women have the resources to push through it.)
Having there be even more long haulers out there than we thought? That’s pretty scary.
Treatments
This article about this paper from the Canada, Brazil, and USA says that a random clinical trial of pegylated interferon lambda, delivered as one shot to people who tested positive for COVID-19 in Brazil and Canada, cut the chance of having a severe outcome (including hospitalization or death) by about half, with basically no side effects! I noticed this drug candidate almost two years ago, and am glad to see the Phase 3 trials are done.
Canada might get this treatment before the US. The FDA won’t approve anything that hasn’t undergone testing on Americans. (This is not as jingoistic as it sounds. This article says there are actually a lot of papers which show that patients treated with ivermectin did better than those without — in places with lots of a certain kind of parasites! Apparently treatment with corticosteroids (like dexamethasone, which is now part of standard COVID-19 treatment) reduces humans’ defences against parasites, and the parasites then wreak havoc. However, ivermectin didn’t work against COVID-19 in the USA because very few Americans have that kind of parasite!)
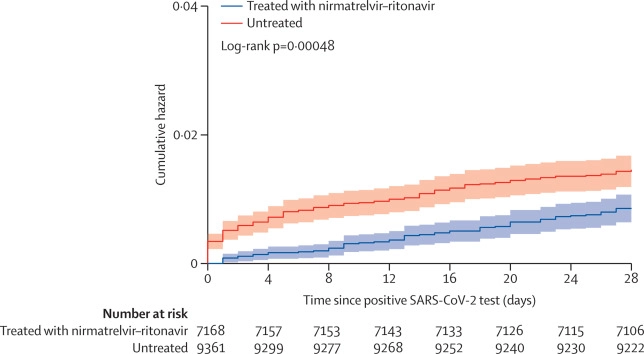
This article discusses this paper from Canada, which found that Paxlovid gives about the same relative/percentage risk reduction of severe COVID-19 for all age/vax groups. However, since young immunocompetent vaccinated people have a much much muuuuch lower risk of severe COVID-19, it maybe doesn’t make economic sense to give Paxlovid to young immunocompetent vaccinated people. (I have seen that the risk of severe outcomes is exponential with age, but I’m not going to bother to look up the reference for you, sorry.)
The study found that the number needed to treat (NNT) to avoid one case of severe COVID-19 was only 28 in unvaccinated people (of any age) and 45 for those over 70, while the NNT was 181 for those under 70. (The paper did not report what the NNT was for unvaccinated people over 70, but it’s got to be really low!)
This article from 2021 reported that the average cost of treating a COVID-19 patient in hospital in BC was CAD$23,000. This article says that the US is paying USD$530 (CAD$704 at today’s rate) per dose; that means that the average hospitalization costs 32 times the treatment cost. That suggests that, from a purely financial standpoint, it’s worth it to treat unvaccinated people, but it’s not even cost-effective to treat people over 70! (For the record, I personally do not think finances are the only reason to give treatments.)
NB: this study was pre-Omicron, and the financial calculation was only for hospitalization, not Long COVID. (Other studies have found that Paxlovid drops the risk of Long COVID by about a quarter.) So there’s still some handwaving and guesswork happening research needed.
This paper from Hong Kong found that there was basically no difference overall in Paxlovid rebound among hospitalized people. They did find that Paxlovid rebound was different in different subgroups, however. The chances of rebounding were:
- About three times more likely for people under 65 than for people over 65;
- About six times more likely people for with lots of comorbidities than for people without;
- About 7.5 times more likely for people who were also taking corticosteroid (of which I think dexamethosone, part of standard severe COVID-19 case, is one);
- About 84% lower(!) for unvaccinated people than for vaccinated people.
The paper noted that people had the same overall disease outcome (how long it took to fully recover, whether they needed hospitalization, etc.) regardless of whether they did/did not rebound.
This paper from USA found a 55% reduced risk of hospitalization and 85% reduced risk of death for patients given Paxlovid.
This paper from the USA looked at extracts from a ton of different plants, and found that extracts from daisy flowers and fern rootstems had potent anti-COVID properties. (Don’t run out and go eat daisies! There haven’t been dosing / safety studies on daisies! These elements will need to be extracted/purified/tested, I’m just alerting you to more potential treatments in the pipeline.)
Vaccines
This paper analyzed blood from a Phase 1 trial in Thailand of NDV-HXP-S and found that it had higher levels of neutralizing antibodies than Pfizer. NDV-HXP-S is hugely interesting to me for two reasons.
- It’s made the old-fashioned way, incubated in chicken eggs. That means that it is really easy to make and really cheap.
- It uses the “HexaPro” spike stabilization. The spike protein has two conformations, open and closed. In SARS-CoV-2, it doesn’t open up until right before it enters the cell. Most vaccines make spike proteins which are not attached to anything, just floating around free — and they sort of flop around and sometimes flop into the “open” configuration. That means that the immune system makes a fair number of antibodies that attach to the “open” form… which is pretty much useless against SARS-CoV-2 except at the very last second. The HexaPro modification to the vaccination spikes’ genetic code keeps it from flopping around as much, so it doesn’t make the worthless “open” configuration antibodies.
The paper found that NDV-HXP-S neutralized SARS-CoV-2 at levels similar to Pfizer. They found that the proportion of antibodies which were neutralizing (i.e. useful) was higher in blood from NDV-HXP-S-vaccinated people than from Pfizer-vaccinated people — which is what you’d expect/hope from a vax which has fewer flopped-open spike proteins.
Something else that the paper found was that the NDV-HXP-S antibodies seemed to focus on the receptor binding domain (RBD), which is the exact piece which plugs into the human cell receptors to let the virus in, than the Pfizer vax does. This might sound like good news, but I think it’s not: the RBD is where the bulk of mutations happen. That suggests that NDV-HXP-S would be really good at the specific strain that it’s targeted to, but not as good against variants. Indeed, that’s what this paper shows: 10 µg of NDV-HXP-S (yellow) does better than Pfizer (purple) at neutralizing COVID Classic, but it’s not as good at neutralizing Delta or Beta.

This makes me wonder if in the future, we’ll take different brands/types of COVID-19 vaccines: one to give specific protection against what’s circulating now, and one to give broader but weaker protection. This makes me feel good about my personal strategy to get diversity in shots (five different shots from four different vendors!).
A word of caution: this paper used blood samples that they happened to have on hand; it was opportunistic and not planned. That means that it was a little less rigorous than other studies. The authors say that it should be taken as “hypothesis generating” and needs further studies to confirm.
This paper from Canada found that vaccinating pregnant mothers protected their babies quite well:
| Against what? | # mom shots | infection VE | hospitalization VE |
| Against Delta | 2 | 95% | 97% |
| Against Omicron | 2 | 45% | 53% |
| Against Omicron | 3 | 73% | 80% |
| Against Omicron, second dose in first trimester | 2 | 47% | N/A |
| Against Omicron, second dose in second trimester | 2 | 37% | N/A |
| Against Omicron, second dose in third trimester | 2 | 53% | N/A |
| Against Omicron, <8 weeks post-birth | 2 | 57% | N/A |
| Against Omicron, >16 weeks post-birth | 2 | 40% | N/A |
Pathology
This paper from China says that almost 40% of patients who had been hospitalized early in the epidemic and who had chest CT scans from that time still had interstitial lung abnormalities after two years.
This paper from Japan found differences in male and female responses to COVID-19. Specifically, there is one type of regulatory T-cell which men lose faster than women. I don’t understand all of the science, but am encouraged that they are making progress. Not only might it help men, but it is likely to give insights at how to treat the disease.
This paper from USA/UK/Chile found that people who ate better had fewer and less severe COVID-19 infections. Adjusted for sociodemographic factors, comorbidities, smoking status, physical activity, and sleep duration, people who were in the top quintile for good diets had a 10-17% lower risk of COVID-19 infection, and a 43% lower risk of COVID-19 death. About a quarter of the risk came from being overweight. (What does “better diet” mean? Read the article.)
Transmission
This paper from the USA found that universities did not cause COVID-19 cases to go up. Counties which had universities actually had slightly lower COVID-19 rates. The authors put it down to universities taking good measures, but I wonder if it was also due to universities being more liberal. (More conservative counties in the US have higher COVID-19 rates.)
There are also existence proofs of COVID-19 going way out of control despite mitigation measures, for example at the University of Illinois in fall 2020.
Recommended Reading
This article talks about current thoughts on Long COVID.
This article by a long hauler talks about Long COVID etiquette.
This article talks about COVID-19 reinfections.
This article talks about how common it is for viruses to spill over from animals to humans, and how that might actually be a good thing. 🤯
