COVID-19
Long COVID
AGAIN 😞 This article (2025-02-04) refers to this paper from the USA (paywalled, 2025-02-03), which reports that 1.4% of children surveyed had had Long COVID, and 0.4% currently have Long COVID. 80% of the kids with active Long COVID have an ability limitation that they didn’t have before catching COVID-19.
They also found that kids from lower socio-economic backgrounds were at higher risk of Long COVID than wealthier ones. 😞
🤔 This preprint from Sweden (2025-02-04) reports that people with Long COVID had a lot more expressed Epstein-Barr Virus than controls.
🤔😕 This paper from Italy (2025-02-04) concludes that getting vaccinated doesn’t change your risk of getting Long COVID if you do catch COVID-19. Note, however, that the study required an in-person visit. That means that the with the worst Long COVID weren’t counted at all in this study. They also didn’t look at how long it had been since vaccination; it is my belief that the time since vaccination matters. (I can’t quote a study off the top of my head right now, and it’s Friday night and don’t feel like looking hard.)
They did find that unvaccinated people had more neuropsychiatric issues than vaxxed, and vaxxed had more cardiorespiratory issues.
There have been other papers which report no association between vaccination and Long COVID. This paper from USA (2024-08-28) used electronic records and not in-patient visits, but they also did not look at how long it had been since vaccination.
This paper from USA (2025-01-07) is relatively recent and articles about the study tend to say that “they found that vaccination doesn’t help”… but I have a real problem with the paper. They split people who had neurological Long COVID symptoms into four buckets: hospitalized/not hospitalized crossed with infected before vaccinated / infected after vaccinated. They found differences in what kind of neurological symptoms people had depending on if they got sick pre-vax or post-vax, but they didn’t find any quality of life differences.
Again, they didn’t distinguish between a recent vax and an old vax… but it seems like the differences they were looking at were not useful for answering the question, “does vaccination help Long COVID?” In this study, they compared one group of people with Long COVID to another group with Long COVID; they didn’t look at vaxxed and unvaxxed people and ask how many got Long COVID and how many did not.
It’s sort of like looking at people hospitalized after car accidents and asking if the people wearing seatbelts were less injured: they are in the freaking hospital! They are in the hospital because their injuries were serious! That framing misses all the people whose car accident injuries were mild enough (because of seatbelts, perhaps!) that they didn’t go to the hospital!
Meanwhile, this paper from USA (2024-07-17), this paper using data from UK and Spain (2024-01-24), and this paper from USA (2024-03-08) found that vaccination did reduce the Long COVID risk, sometimes by a lot. 😕
😞 This paper from USA (2025-02-07) reports that kids who had confirmed COVID-19 infections had higher rates of gastrointestinal issues than controls. Kids who’d had COVID-19 had about a 25% higher risk than controls of developing a GI problem 28 to 729 days after the acute infection. They had about a 14% higher risk of abdominal pain in the 28-179 day post-acute phase and a 24% higher risk of abdominal pain in the 180-729 day chronic phase.
COVID-Related Excess Deaths and Sickness
😞 This paper from Türkiye (2025-02-01) reports that people who had had COVID-19 infections had dramatically higher risk of having autoantibodies (i.e. antibodies to parts of the person’s own body) than controls (who had never had a positive PCR test or COVID antibodies in their blood) — 48.5% compared to 19% in healthy controls. They also found:
- 2/3 of the people with high autoantibodies — both recovered from COVID-19 and healthy controls — were women.
- The historical rate of autoantibody positivity in Türkiye is around 2-15% in healthy controls, but this study found a rate more like 15-20%. This percentage has been rising over time; they didn’t guess as to why.
😞💀 This paper from USA (2025-01-31) reports that excess deaths in young adults (25-44 y/o) was 70% higher in 2023 than you would have expected if trends from 2011 had continued. These five causes of death accounted for almost 75% of the young adult excess mortality:
- drug poisoning (31.8%);
- “the residual natural cause category” (16.0%);
- transport-related deaths (14.1%);
- alcohol-related deaths (8.5%);
- homicide (8.2%)
Cardiometabolic conditions combined accounted for 9.2% of excess deaths.
😞 😞 This paper from China (2025-02-04) reports that atherosclerotic plaque grow roughly a third faster (depending on which measurement you use) in people who’d had COVID-19 infections than those who had not.
😞 This paper from Egypt (2025-01-31) reports that two years after being discharged, more than half of the people who had been hospitalized with COVID-19 had abnormal thyroid levels. 46.5% were being treated for hyperthyroidism; 10.1% were being treated for hypothyroidism.
Transmission
😬🐈🐕 This preprint from USA (2025-02-04) reports that almost 30% of household pets (almost all dogs or cats) had evidence of past or active COVID-19 infection. 39% of households with pets in the study had at least one companion animal with evidence of past or active COVID-19 infection. 😞
Cats were more susceptible than dogs, with 13.4% of cats actively sick and another 36% had COVID-19 antibodies, while only 4.8% of dogs were actively sick and 25% of dogs had antibodies. 😞
Pathology
AGAIN This paper from Brazil (2025-01-31) reports that the risk of death or ICU admission was about seven times higher for pregnant women who had COVID-19 infections than those who did not. The risk of any severe maternal outcome was about six times higher for women with COVID-19 than women without. All of the women who died were unvaccinated. 😞💀💉
😞 This paper from USA (2025-01-30) reports that children who had COVID-19 infections were almost six times more likely to get a new psychiatric diagnoses than healthy controls. For adolescents, the psychiatric diagnosis risk was similar after COVID-19 than other respiratory infections (!), but for children the risk was 57% higher.
(I didn’t know that flus and colds made psychiatric diagnoses go up, let alone by that much!)
🤔 This paper from Qatar (2025-02-05) reports that COVID-19 infections pre-Omicron gave pretty durable protection against pre-Omicron variants, but after Omicron, infections became way less durable.
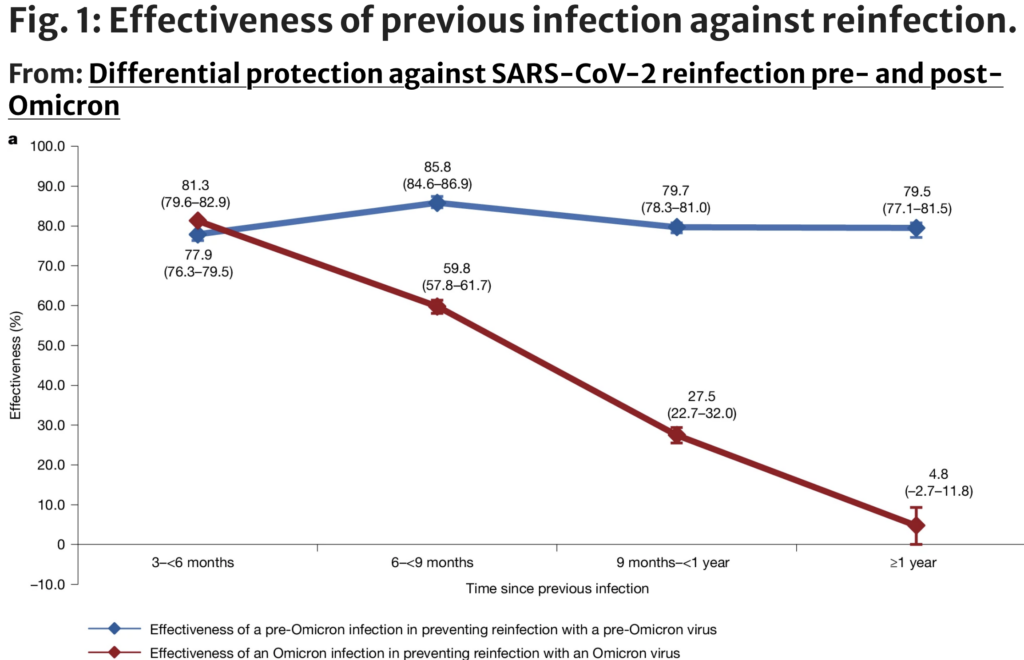
Pre-Omicron was defined as between 5 February 2020 to and 18 December 2021; post-Omicron was between 19 December 2021 and 12 February 2024.
This dramatic decrease in the effectiveness of a prior infection against a second infection shows up even if you only look at vaccinated people or only look at unvaccinated people.
I am surprised by how good infections used to be for preventing future infections, and don’t quite know what to make of it. I believe it’s in conflict with other studies, but pre-Omicron is now a long time ago and I don’t have studies I can instantly call up.
Vaccines
🎉 This paper from Italy (2025-02-04) reports that getting multiple vaccine doses reduces the risk of a neurological disorder after a COVID-19 infection by 86% for people over 60 years and 96% for people with comorbidities.
Side Effects
😞 This article (2025-01-30) reports on a survey about friendships of people with Long COVID and people still taking COVID-19 precautions. 81% reported having lost friends over the course of the pandemic.
H5N1
Variants
This press release from a branch of the US Department of Agriculture (2025-02-05) says that their milk testing found a dairy herd in Nevada which is of clade 2.3.4.4b, genotype D1.1. This is the first time they’ve found D1.1 — which is the variant that birds usually have, what the BC teen who had bird flu had, and what the Louisiana fatality had — in US dairy herds. The infected USA cows always had genotype B3.13 before.
As this article (2025-02-05) about the press release says, that means that bird flu has jumped to cows at least twice — meaning that it’s going to be harder to control in cows than we had hoped. It’s looking like we’d have to eliminate it from wild birds, not just domestic cows. 😬 And if there are two variants infecting cows, then any H5N1 cow vaccines will have to be extra good. 😬😬
On the other hand, yay for the US bulk milk testing finding an infection!
Transmission
🐄 This article (2025-02-06) reports that the US H5N1-infected dairy herd count is up to 950, with 738 in California.
🐓🥚🪿🐣🦃 I haven’t talked a lot about bird flu in birds because it’s not really news — birds have been getting H5N1 for years. However, the pace of infections has been pretty relentless lately.
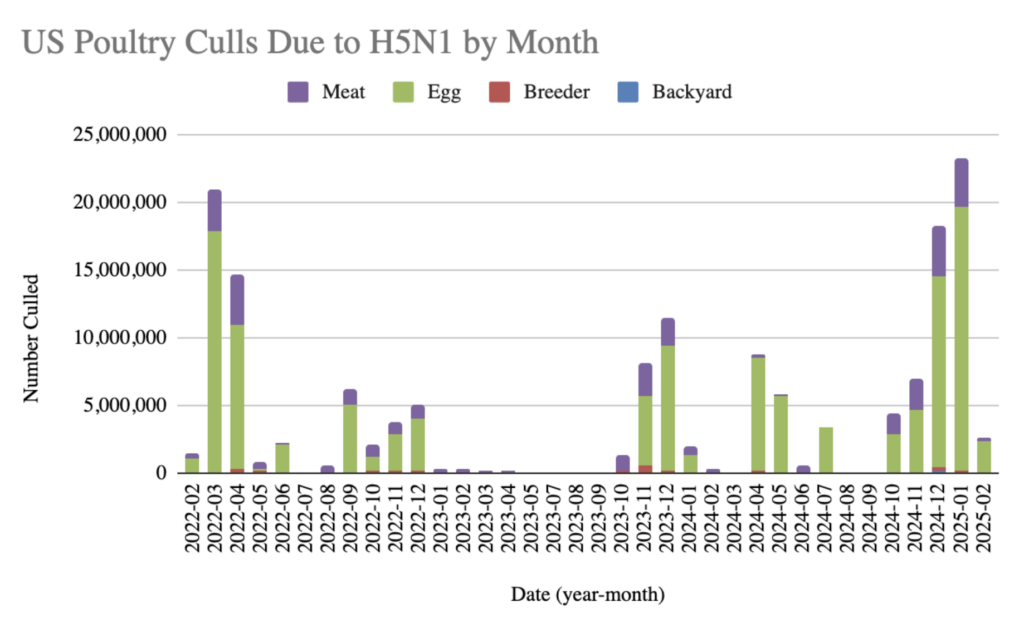
Surprisingly, I had to make this graph myself (including me scraping and Favourite Spouse cleaning the data) because I couldn’t find one. Does nobody care, are my search techniques crappy, or did everybody else think that the graph just wasn’t that interesting?
This article (2025-02-06) reports that information about a bird flu-infected cat possibly (probably?) infecting a human appeared briefly in a US CDC report before hurriedly getting pulled down. ❓❗❓❗❓I assume this is Trump Musk shenanigans.
This paper (2025-01-30) was a bit hard for me to understand, but I think it says that pasteurization might not kill all the H5N1 in milk. (Explanation below.) I am not actually all that worried about my milk, partly because I live in Canada, but also because we know that some infected milk has made it into the supply in the USA — multiple cats have died from drinking raw milk! — and yet we haven’t seen a lot of people dying in the US from drinking milk. Yes, there are two or maybe three people in the US who have unexplained H5N1 infections, but it seems to me like there would be more if this was a serious problem. (NB: It’s highly UNlikely that the Fraser teen got bird flu from milk because 1) she lives in Canada and 2) she got the bird variant of H5N1 and not the cow variant of H5N1.)
Okay, the explanation: it turns out that in a viral infection, there are a lot of virus-like things — tiny particles — that don’t show up on the standard tests for virus particles which infect cells — but they are there nonetheless. Those are called “non-infecting particles”, and they don’t seem to be well understood. Some of them are clearly “helper” cells; I suspect that some are basically decoys. I read one paper which thinks they are active viruses which just weren’t “good enough” to succeed at infecting something, so didn’t get counted in the standard tests. Those are called “non-infectious”. Hold that thought.
This snippet’s featured paper says that influenza virus particles have two forms. One form (called HA0) has an HA protein (which helps get the virus into cells) that is intact and one form has the HA cleaved into two pieces (HA1 and HA2). The paper says that the particles with HA0 (intact) can’t get into cells, but the ones with separate HA1 and HA2 can. The HA0 is thus “non-infectious”.
However, this snippet’s paper and this other old paper (2019-10-22) say the HA0 can get cleaved by trypsin (which I understand is a normal thing just floating around the human body) and thus become infectious.
This snippet’s paper also say that pasteurization kills the infectious particles — the ones with HA1 and HA2 — but that the particles with HA0 are more resistant to pasteurization.
Put that all together, and this snippet’s main paper seems to be saying that pasteurization will kill of a ton of all of the currently actively dangerous virus, but there are still a bunch of sneaky particles running around that can turn into active virus particles. Ulp if that turns out to be true. 😬
Treatments
🎉 This paper (2025-01-30) reports that researchers found a monoclonal antibody — MEDI8852 — that can protect macaques from catching H5N1 prophylactically.
Recommended Reading
This long article (2025-02-07) talks about how hard it has been for US egg producers: all the things they have done, how it isn’t working, and what measures they are considering. (From last week’s General post, this article implicitly points out that a lot of the problem is ginormous poultry farms are in the US.)
Sudan Virus
Transmission/Vaccination
You might have seen articles like this one (2025-02-01) saying that there has been an Ebola outbreak in Uganda. 😞💀 That’s not exactly wrong but not exactly right: this press release from WHO (2025-02-01) says it’s the Sudan Virus (Sudan ebolavirus) — a relative of the Ebola virus. Unfortunately, talking about the Sudan Virus in Uganda is confusing, and it is in the ebola family, so news outfits are frequently calling it plain old “Ebola”. Whatever.
The wikipedia article on sudan ebolavirus says that its symptoms are just like Ebola (bad! 💀), but it’s less transmissable (good! 🎉).
The good news is that this article (2025-01-31) says that WHO has already sent candidate vaccines. 🎉💉 These vaccines are part of a “vaccine trial”, so haven’t been approved yet, but sadly/happily this outbreak could help get them approved.

1 comment
Comments are closed.