Long COVID
This paper from USA looked at Long COVID in US veterans over two years. It found:
- While the number of people with Long COVID symptoms decreased over the course of two years, there were still a lot of people with symptoms after two years.
- There were not a lot of excess deaths after six months in people who had not been hospitalized when they had COVID. However, death rates were elevated over the whole two year period for those who had been hospitalized.
- The people who had been hospitalized had much higher rates of symptoms for most types of symptoms.
Note, however, that this study did not look at the risk of diagnoses of other illnesses, e.g. diabetes, cardiovascular incidents, neurological impairments, etc. which other studies have found.
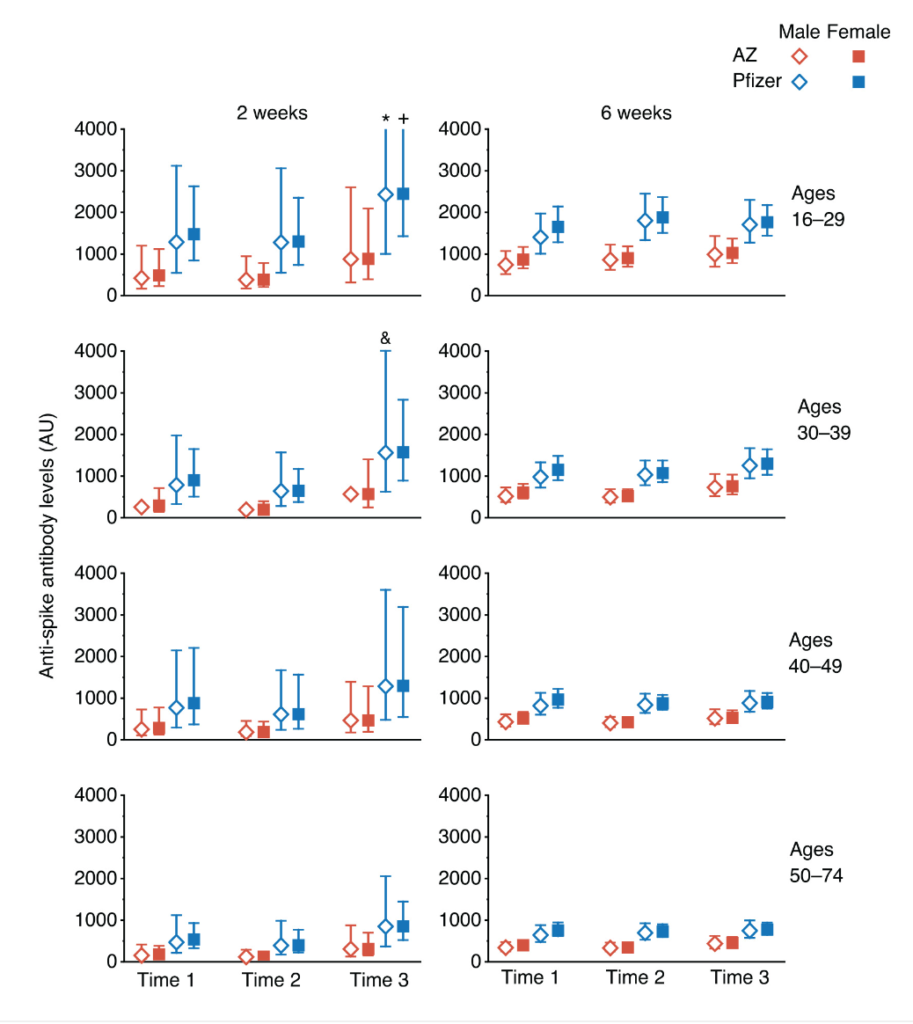
Also, this study was done on US veterans, an 90% male population, while long haulers are overwhelmingly female. This study from Norway shows that recovery trajectories are very different for men and women. Basically, men recover more than women for most impairments:

This paper from UK found that there were two different sets of acute-phase biomarkers which predict if a patient will have brain fog six to twelve months later. One of the markers predicted brain fog only; the other predicted brain fog plus fatigue.
This paper from Hungary reports that elite aquatic athletes who were surveyed at a World Championship found that 10% of those who got COVID-19 got Long COVID.
My reaction was “see, even healthy young people can get COVID-19!” and someone pointed out that elite athletes aren’t always “healthy” — that elite athletes push their bodies in uncomfortable ways to their limits.
Note, however, that they had a very low bar for their definition of Long COVID: “symptoms that persisted beyond 4 weeks after the start of the infection”. (Presumably if they had really bad Long COVID, they wouldn’t have made it to the World Championship.)
This report from the US found that 18.9% of non-institutionalized adults who had prior COVID-19 infections had Long COVID as of June 1–13, 2022, but that fell to 11.0% during June 7–19, 2023. A quarter of the long haulers reported significant activity limitations.
This paper from Germany reports that Long COVID patients fall in two categories: those who fit the criteria for ME/CFS and those who did not. They found that the ones without ME/CFS-matching symptoms pretty much got better over twenty months while those who matched ME/CFS symptoms pretty much didn’t. They also found that hand grip strength at the onset correlated with the severity of symptoms.
Good news! This paper from Sweden found that the risk of Long COVID have been going down. Compared to Omicron, the risk of getting Long COVID was 3.26 times higher for Delta, 5.33 times higher for Alpha, and 6.31 times higher for COVID Classic.
COVID-Related Excess Death and Sickness
This paper from USA found that the all-cause mortality for COVID-infected veterans between March 2020 and April 2021 was six times that of non-infected veterans in the first three months of infection. It was ~20% higher in months 3-6, and actually slightly lower from six months to two years. This is probably due to the most vulnerable dying earlier than they would have without COVID-19.
Some good news! This paper from Netherlands found that in a group of elite athletes, 3% had MRIs which suggested myopathy (muscle fibres not functioning properly), but all of them returned to elite-level competition within 26 months. None of the athletes had to drop out of elite-level competition due to COVID.
Aaand back to bad news: this paper from USA found that people who had COVID-19 were more likely than uninfected controls to develop high blood pressure which was persistent for at least six months. People who had not been hospitalized were 52% more likely to get high blood pressure than controls; people who had been hospitalized were 2.23 times as likely to get hypertension.
Vaccines
I mentioned this when the preprint came out, but it seems important enough to mention again (especially since Jeff reminded me of it!): this paper says that COVID-19 vaccines were more effective if they went into the same arm vs. the opposite arm.
This seems like a good time to remind people that vaccines given later in the day are more effective than ones earlier in the day, according to this paper. It looks like you should try to get an evening shot!
The nasal vaccine BBV154 (also called iNCOVACC), which has been approved in India for almost a year elicits much better IgA responses to COVID Classic than the (intramuscula) COVAXIN. They gave similar IgA responses to Omicron, but BBV154 reached interesting levels faster.

The intranasal vaccine also had fewer side effects.
This paper from USA found that how effective vaccines were depended on the amount of virus that people were exposed to. In a clever study of vaccinated prison populations, they found that transmission was highest when a prisoner shared a cell with someone infected; next highest when a prisoner shared a cellblock with someone infected; lowest when there was no cell/cellblock exposure. This was true regardless of whether the prisoner’s immunity was from infection-acquired immunity, vaccination-acquired immunity, or hybrid immunity.
| Proximity | infection | vax | hybrid |
| Shared cell | 36% | 57% | 24% |
| Shared cellblock | 61% | 69% | 41% |
| Other cellblock | 89% | 96% | 80% |
For example, vaccination was 96% effective at keeping prisoners from getting COVID-19 from somewhat more casual contact with the general population (presumably from passing in the corridors or in the yard), but only 57% effective from the more intensive exposure of sharing a cell.
This paper from Sweden found that higher cognitive abilities (as measured by the military intake tests, which are linked to military opportunities among the young men (and women after 1980) entering compulsory service) correlate with getting the COVID-19 vaccine faster.
Treatments
This paper from USA found that Black and Hispanic patients were much more likely to have their oxygen saturation measurements being flawed (because of their darker skin), leading to under-treatment for COVID-19. Black patients were 50% more likely than White patients to have overly-high measurements and Hispanic patients were 18% more likely.
Transmission
This paper from USA found that 4.4% of people in the hospital with COVID-19 caught it there, and in 3.8% they weren’t sure if they caught it in the hospital or not (because they didn’t test those patients on entry, I believe). Even 4% seems like a lot — 1 in 25 people catching COVID-19 in the hospital? I swear, don’t go to the hospital!
This paper from Hungary (also mentioned above in the Long COVID section) found that elite aquatic athletes who they surveyed about previous COVID-19 infections had a lot of variation by sport. The infection rate was:
- 28% for open water swimmers;
- 67% for water polo players;
- 61% for synchronized swimmers.
I observe that most open water swimming is individual (or at best, a relay made up of four people taking turns doing an individual event) while water polo and synchronized swimming are very much team sports.
This paper from Indonesia looked at whether TB infection made you more susceptible to COVID-19 or vice-versa. They found that people with one were less likely to get the other! 28% fewer people infected with COVID-19 got TB than expected; 45% fewer people infected with TB got COVID-19.
Variants
People seem to be freaking out about BA.2.86.
The preliminary information that I have seen says that yes, BA.2.86 has a heck of a lot of mutations on top of some older variant, making it very different from other variants.

However, what little genomic surveillance we have doesn’t seem to say that it’s ZOMG crazy-scary. Yes, it’s spreading… but COVID-19 in general is spreading.
Furthermore, there’s this Twitter thread from Sweden that repots that an infection (and hence likely also a vaccination) with XBB.1.5 gives some useful antibodies against BA.2.86.

On the other hand, this twitter thread from China reports that BA.2.86 evades XBB.1.5 andibodies, but that BA.2.86 is not all that contagious.
And this preprint from USA says that neutralizing antibodies block BA.2.86 at levels comparable or slightly higher than currently circulating variants.
And this twitter thread from South Africa says that BA.2.86 is not that scary.
But this preprint from Japan says that BA.2.86 is highly evasive.
You can look at this blog post to get a more detailed look at all the recent research on BA.2.86.
So sure, you can keep an eye on BA.2.86, but I don’t think it’s worth panicking yet. Well, any more than you’re already panicking about COVID-19 in general, which probably isn’t very much.
This preprint from USA/Moderna found that the new Moderna XBB.1.15-based vaccine does a credible job against BA.2.86 (as measured in donor blood in test tubes). It’s not totally awesome fantastic, but it’s not bad:

Pathology
This paper from Canada found that 1 in 8 older adults with no prior symptoms of depression got an initial depression diagnosis. Those who had cancer and a history of depression had ~a 50% chance of getting depressed again. Older people who were lonely and didn’t have enough money were more likely to get depressed. (<- These all seem like very reasonable things to me to be depressed about.) It was 50% worse for women because of course it was.
This paper from Canada says that delirium increased by 15% during the pandemic, yet the prescription of anti-psychotic drugs increased by 22%. This opinion piece by the authors of the paper say that delirium is reduced if family members are present, patients get some exercise (or at least move around a bit), and have fewer disruptions to eating/drinking/sleeping. The first two would definitely have been disrupted by the pandemic restrictions.
Recommended Reading
This blog post is a nice lay discussion of some of the Long COVID pieces I mentioned above.
This article goes in-depth COVID-19’s effect on heart health.
