Long COVID
As a reminder that Long COVID is a real problem, this report says that 2.4% of people in the UK report Long COVID symptoms more than four weeks after infection. Not 2.4% of the people who got Long COVID, 2.4% of ALL the people. Of that 2.4%, 45% (i.e. 1.08% of the total population) report symptoms for more than a year. Long COVID is a BFD and you really should try not to get COVID.
This article talks about a small but noticeable number of cases of people having psychotic breaks after a COVID-19 infection.
Vaccines
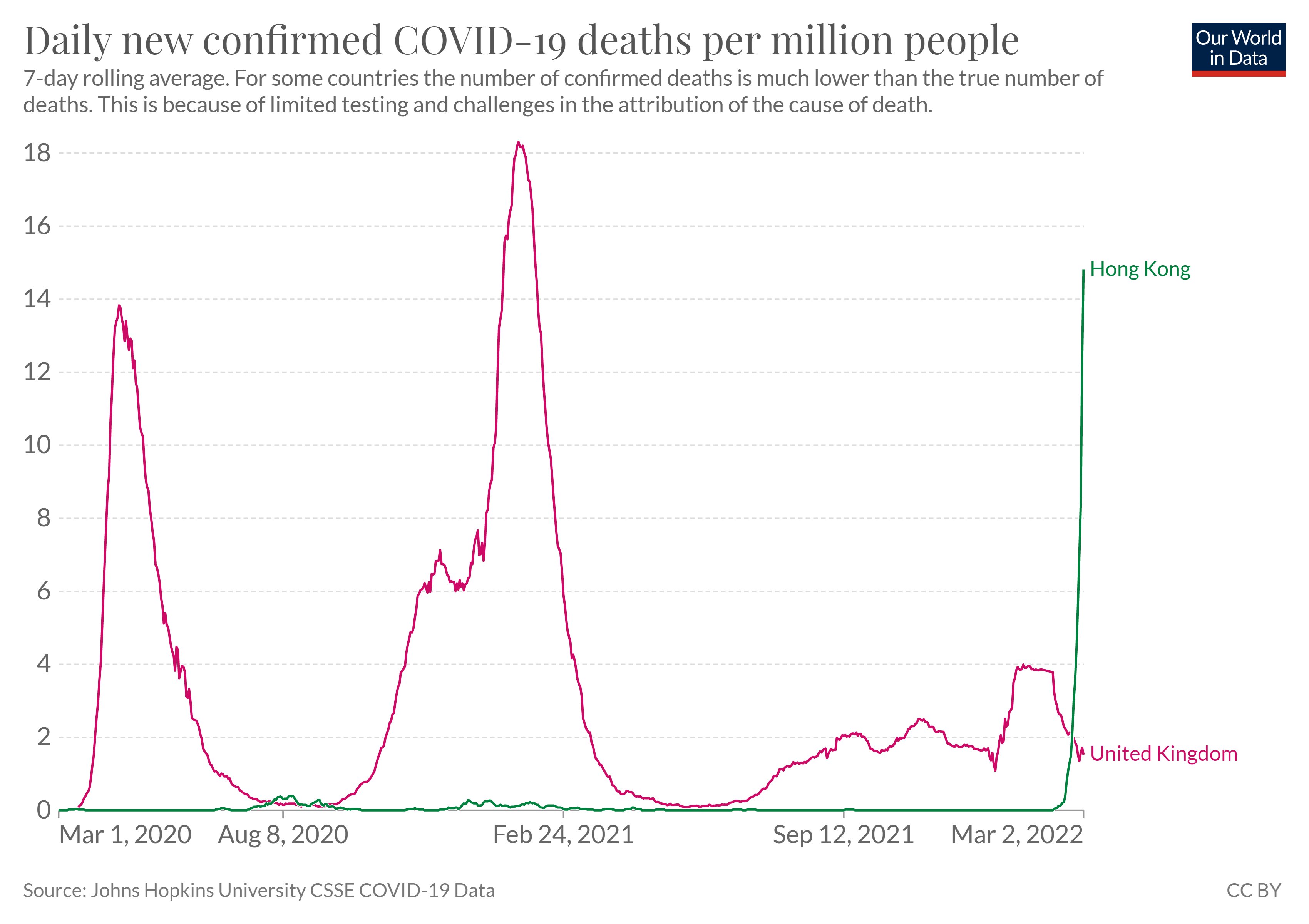
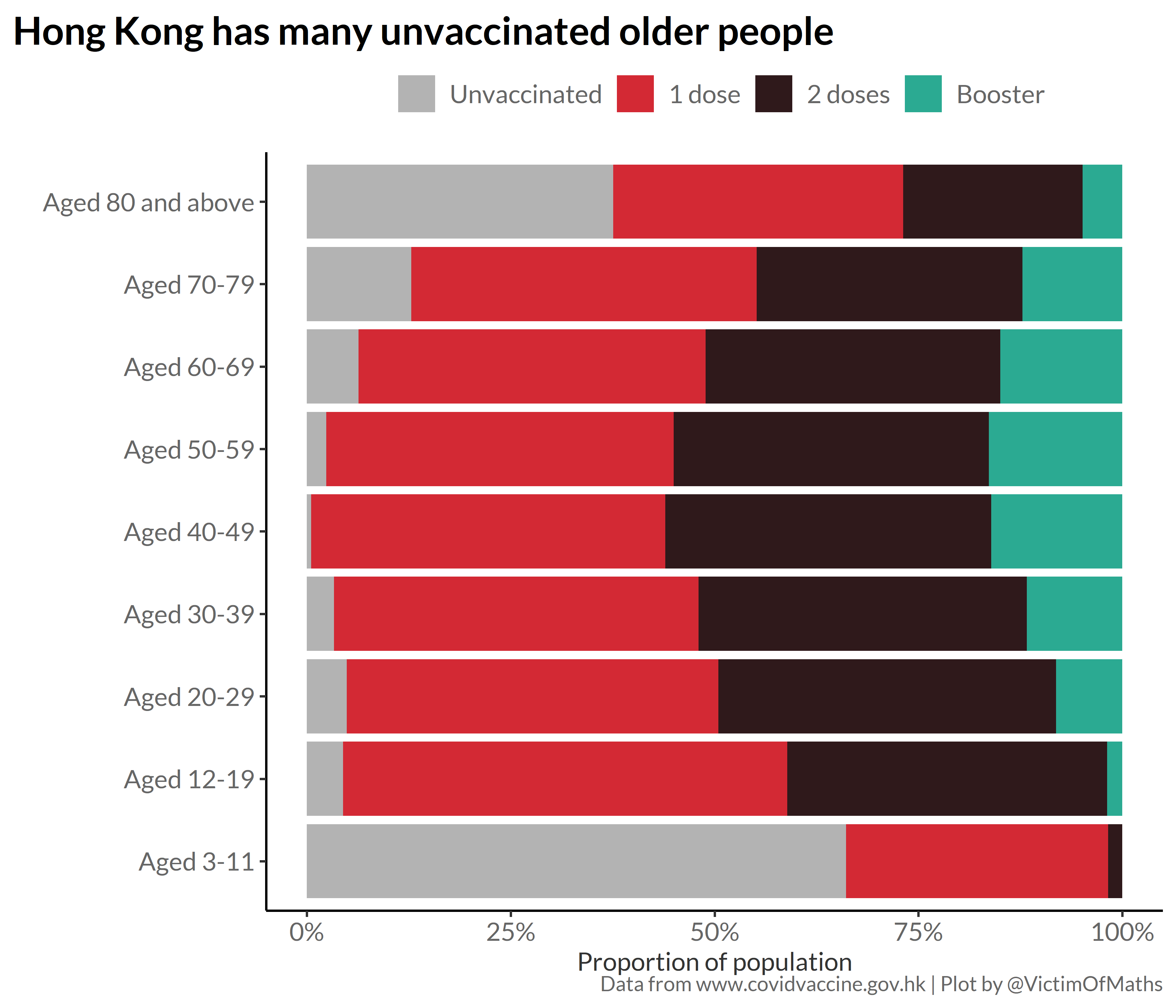
“Omicron is mild”, right? It is milder than Delta, but that makes it about as mild as COVID Classic. To get a visceral sense of how virulent Omicron still is, look at the difference between how it is hitting Hong Kong and the UK. The UK has done a much better job of vaccinating (especially with boosters and with the elderly). (Graphs from this tweet.)
Current NZ vaccination by age, from this Twitter thread:
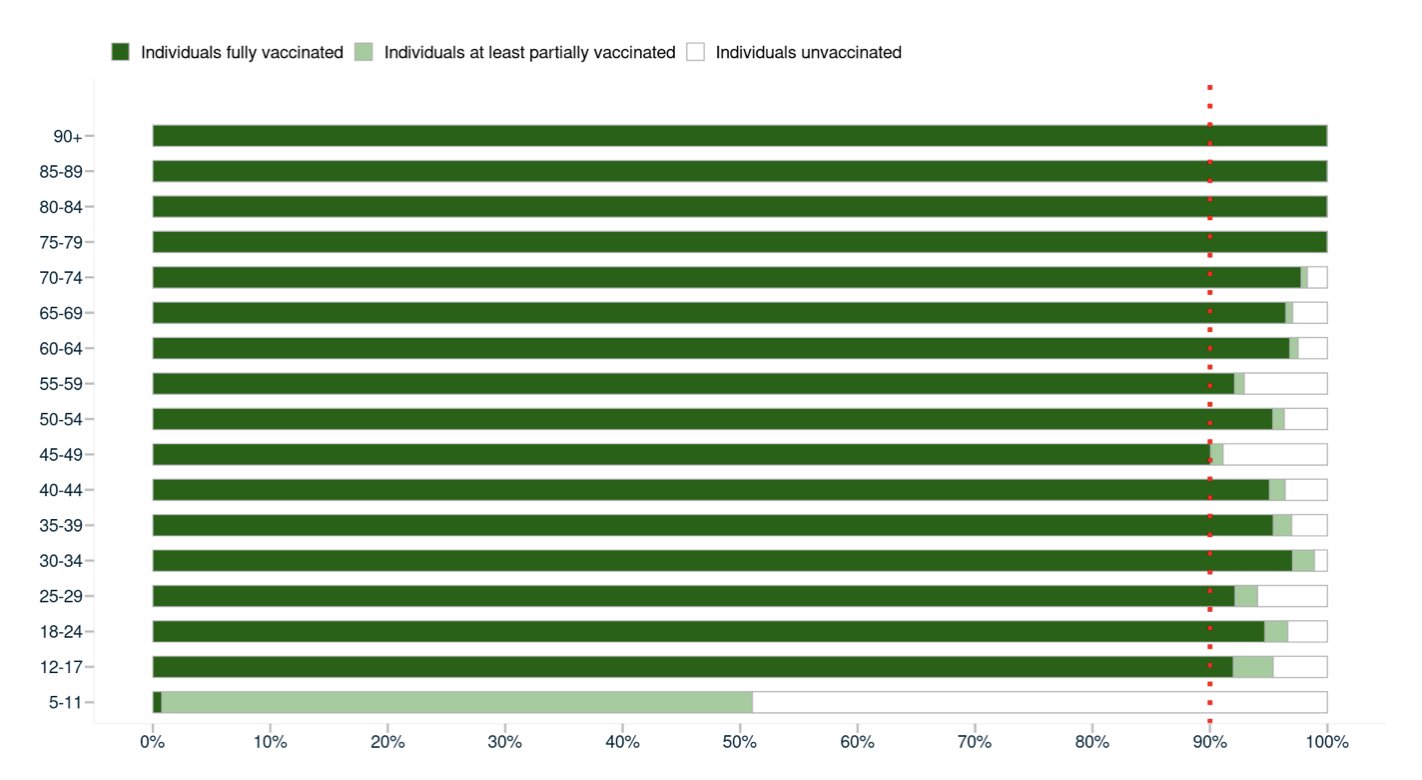
(That Twitter thread and comments also points out that New Zealand mostly used mRNA vaccines, while lots of the vax used in Hong Kong was Sinovac’s Coronavac, which does not work as well, especially against Omicron.)
Pathology
Remember how odd it sounded when, early in the pandemic, they found that smokers were less susceptible to COVID-19 than non-smokers? This article says that better studies found smokers actually were more susceptible to COVID-19.
Variants
This preprint quantifies how much worse BA.1 and BA.2 are than Delta.
| BA.1 | BA.2 | |
| generation time | 0.60x | 0.51x |
| reproduction number R0 | 1.99x | 2.51x |
BA.2 has a generation time which is 0.85x that of BA.1; BA.2 has an R0 which is 1.26x that of BA.1.
This seems like all bad news, but one piece of good news out of it is that the preprint says we ought to be able to reduce quarantine times (i.e. for people who came into contact with an infectious person) by 51% for BA.1 and 60% for BA.2. Of course, nobody is doing any quarantining at all any more 😞, but it’s nice to know.
Treatments
This article reports on a study from Minnesota where they separated patients by COVID status into dedicated COVID and non-COVID hospitals. Results on several metrics were better than for non-split hospitals.
