Long COVID
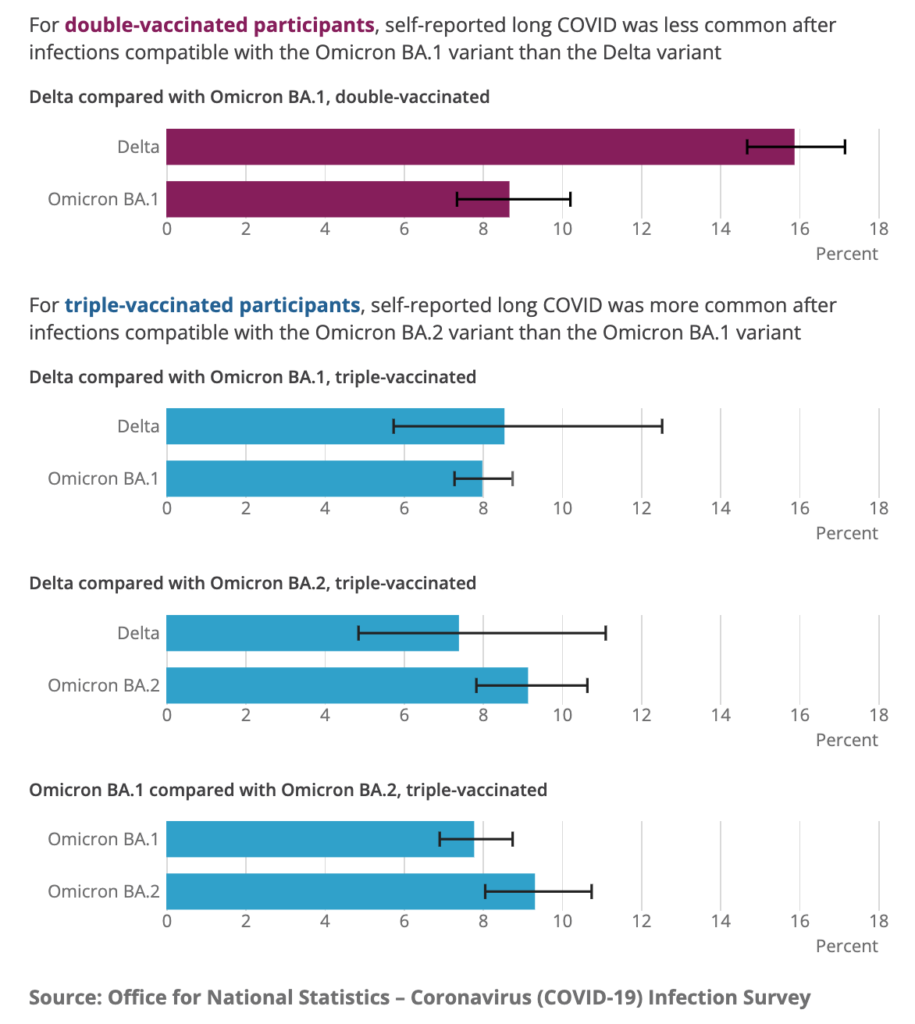
This report from the UK found that double-vaxxed people were almost 50% less likely to get Long COVID after Omicron than after Delta, but triple-vaxxed people were slightly more likely to get Long COVID after Omicron than after Delta.
A different UK governmental report found that 2.8% of the entire UK population self-reports as having Long COVID. Two-thirds say that it has affected their day-to-day activities, and 19% said their activities had been “limited a lot”.
This preprint from the UK and this preprint from the USA both found markers of Long COVID. The first one found a marker which 55% of Long COVID patients with impaired ability to exercise had; the second identified a signature in a bunch of different biological agents. (You don’t need to read the papers, just know that they keep making progress finding Long COVID markers, which has implications for treatments.)
This preprint from South Africa found microclots in the blood of 80 out of 80 Long COVID patients.
This paper from China says that Long COVID in previously-hospitalized patients does get better over time, but how much depends on what kind of symptom. The number of people with at least one symptom dropped from 68% at six months to 55% at two years, which doesn’t seem that great. However, it was a lot better for the percentage with other symptoms going from 6 months to two years:
- depression or anxiety: 26% to 14%
- lung diffusion impairment: 65% to 36%
- reduced residual lung volume: 62% to 20%
- total lung capacity: 39% to 6%
Vaccines
This preprint from South Africa says that Omicron BA.1 infection by itself doesn’t give very good protection against Delta, Beta, or BA.2. However, vaccination + BA.1 infection does give good protection against Delta, Beta, and BA.2.
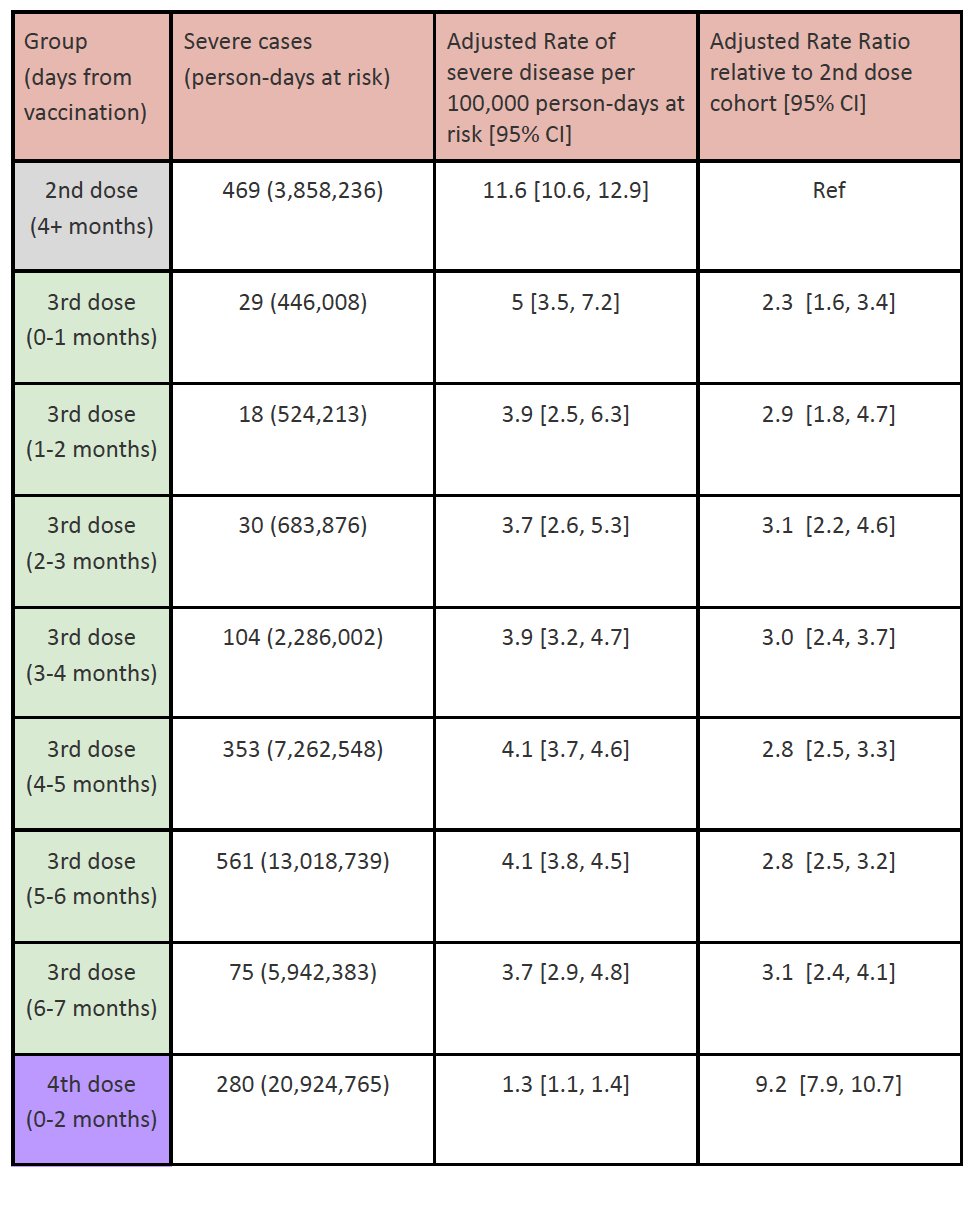
This preprint from Israel says that protection against severe disease from a third dose doesn’t wane very much over the course of seven months.
Variants
This preprint says that when you adjust for confounding factors, Omicron is no milder than other variants.
Treatments
This paper from researchers around the world found that existing monoclonal antibodies didn’t work well against newer strains, but they also found a pan-coronavirus antibody (S2X324) which seems to work really well against all the COVID-19 variants we know about and against at least one pangolin sarbecovirus (though not against SARS-1).
This article talks about people taking Paxlovid, testing negative, finishing the 5-day treatment, and then testing positive again. (There have also been a few case study papers.)
This article talks about a side-effect of Paxlovid: a really vile taste in the mouth.
Pathology
It became clear to me early in the pandemic that people with diabetes were at much, much higher risk from COVID-19 than controls, but I didn’t understand why. This paper says that diabetics have various changes in kidney cells (and possibly elsewhere, but they just looked at kidneys) which include an increased number of ACE-2 receptors — the things that SARS-CoV-2 grabs onto to infect cells. (There are some other metabolic changes in diabetics, but I don’t understand how they interact with SARS-CoV-2. “More ACE-2” is easy for me to understand.)
Recommended Reading
This article talks about why there are no studies of Paxlovid treatment for Long COVID. tl;dr: it’s hard to prove clinical effectiveness for X when you have neither an objective test for who has X nor a test to say when it’s over.
This article says that the lab-leak story was pushed by an animal-rights group masquerading as a anti-government-spending group.
This article talks about the “also-rans”: the variants like Mu and Lambda which died out.
