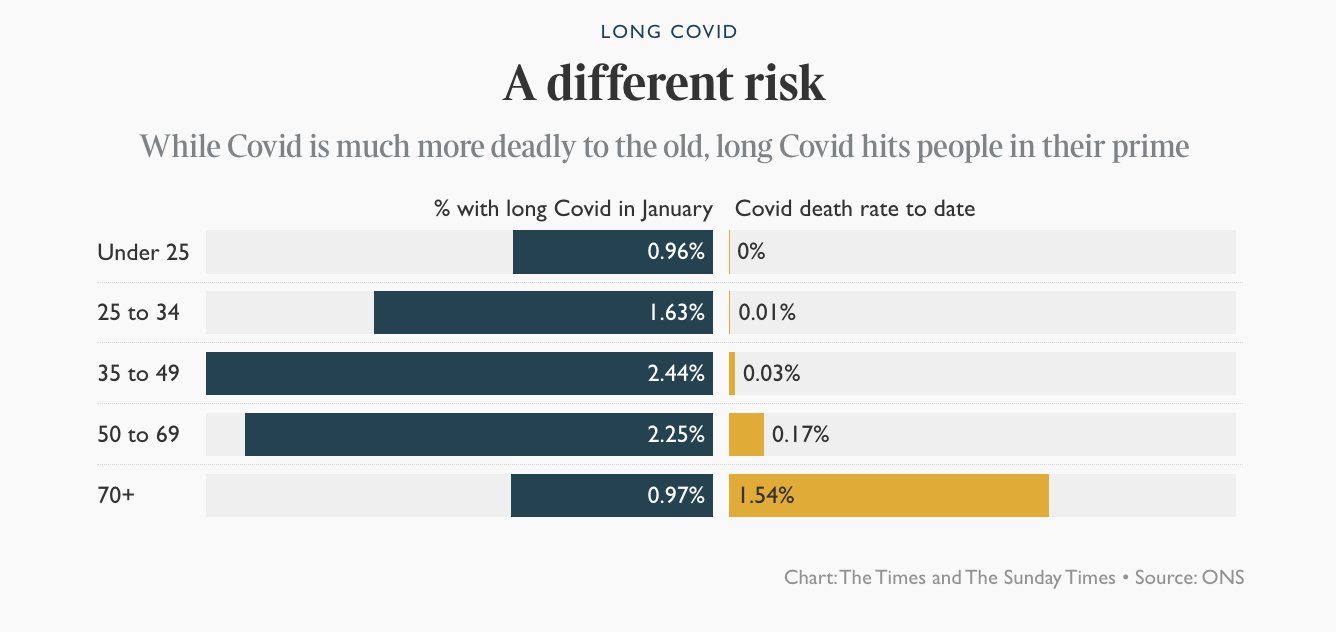
Long COVID
This preprint says that people with Type O blood are 4.2x as likely to get Long COVID as non-O people.
From this Twitter thread:
Treatments
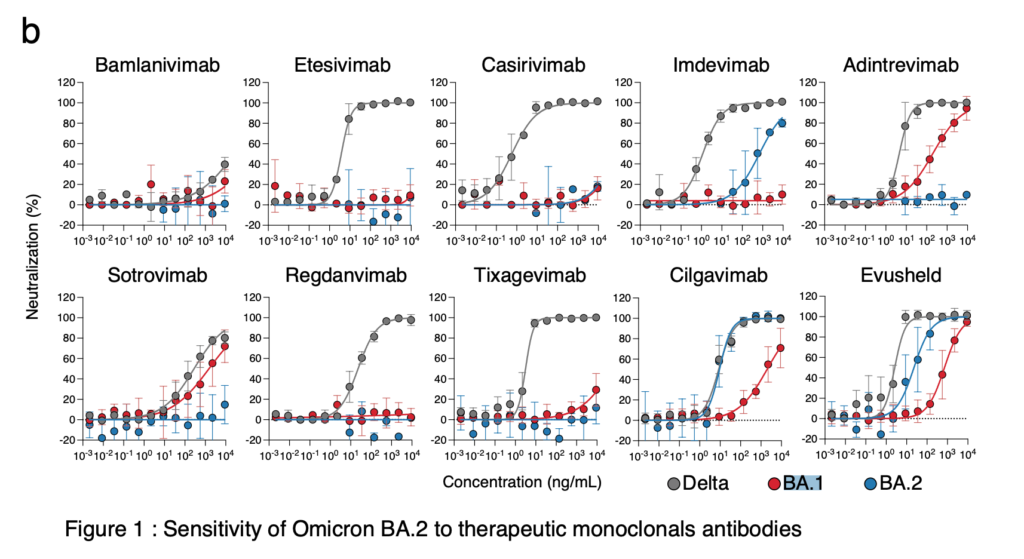
This preprint looked at effectiveness of monoclonal antibodies against BA.1 and BA.2. It is striking to me how well a monoclonal antibody works against one of the strains really doesn’t predict how well it will work against the other.
BA.1: Adintrevimab and Evusheld worked somewhat well. Sotrovimab and Cilgavimab worked, but less well.
BA.2: Cilgavimab and Evusheld (which has Cilgavimab in it) worked really well, and Imdevimab worked, but weakly.
Pathology
This preprint says that SARS-CoV-2 can infect blood cells, including T cells. Furthermore, SARS-CoV-2 does not need the ACE2 receptor to infect the T cells.
Vaccines
This Twitter thread speculates that Novavax is likely to have more broad antibodies than the mRNA vaccines. There are two proteins that make up the spike: S1 and S2. Before the virus enters the cell, the spike is cleaved (at a place called the furin cleavage site) and splits it into S1 and S2. Remember for later: that this happens as part of the cell entry process.
The mRNA vaccines cause your body to make spikes, but according to the thread, it makes cleaved spikes. The thread author thinks that the S1 spike ends up being more prominent, or used more, or something, than the S2. (I believe it is true that most monoclonal antibodies — which are ultimately derived from what people make after being vaccinated — target S1.) Well, the bad news is that a) there are more mutations in S1 than in S2 and b) when the viruses are floating around the bloodstream, their spikes are going to be the full S1+S2 spikes and not the pieces.
Well, the Novavax people disabled the furin cleavage site, so the spikes that get dumped into the body are the full thing. That means that Novavax might give broader antibody coverage, i.e. it might be less bothered by mutations.
The author did find a study which found that some S2 antibodies to some “common cold” antibodies offer protection against SARS-CoV-2 — that’s how rarely the S2 protein mutates.
This is good news! Not only would a more variant-resistant vax help, but they find monoclonal antibodies by looking in the blood of people who have been infected or vaxxed. If more people have S2 antibodies in their blood, that should make S2 monoclonal antibodies easier to find.
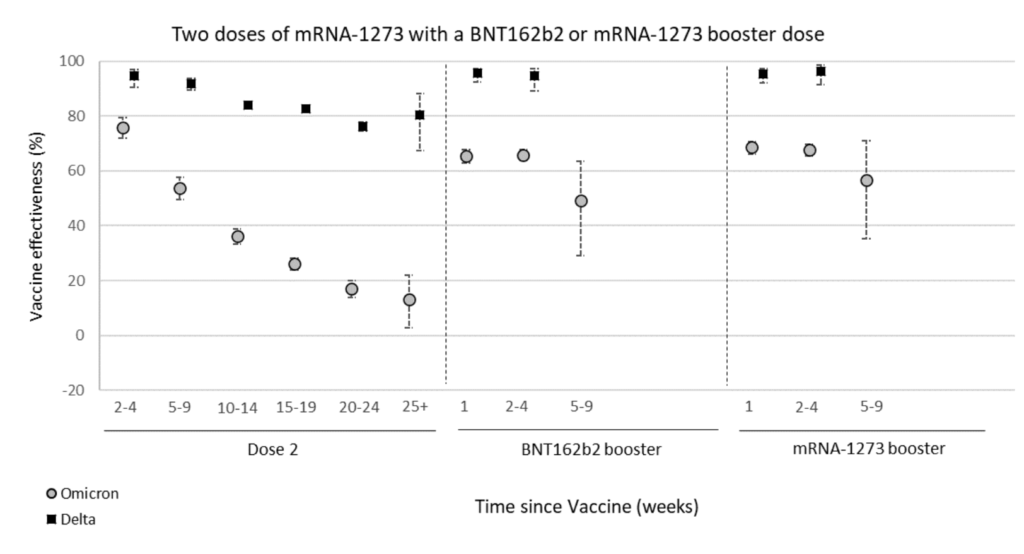
This report from the UK gives an update on vaccine waning:

Side note: If you “Omnivax”, with one dose of AZ, one of Pfizer, and one of Moderna, so I have been carefully for anything which might say how good that combination is. I and my spouse are both Omnivax. So far, I have seen nothing, sorry.
Pathology
This article said that people with ADHD have a 50% higher risk of death from COVID-19 than controls. Someone quoted in the article theorized that people with ADHD would be less able to consistently use personal protective equipment properly or to show up for treatment or testing. Finally, ADHD people are more likely to smoke (self-medication?) and that’s also linked to poor COVID-19 outcomes.
Recommended Reading
This article talks about the early days of making the Pfizer/BioNTech vax.
