This paper from India (20231204) found that a quarter of men who had recovered from COVID-19 infections had low testosterone.
This preprint from USA (20231205) used a very large data set to look at new diagnoses of schizophrenia and psychotic disorders in three groups: those who had acute respiratory distress syndrome (ARDS), those who were COVID-positive but did not have ARDS, and those who were COVID-negative. The COVID-positive group had a WAY higher risk of getting a new diagnosis of schizophrenia or psychotic disorders than either of the other groups, although it went down significantly over time:
| Time | Increased Risk |
| 0-21 days | 360% |
| 22-90 days | 190% |
| over 90 days | 70% |
This paper from Sweden (20231121) found that the risk of cardiac arrhythmias was WAY higher in the first 30 days after getting COVID-19:
| Arrhythmia Type | Times-higher Risk |
| atrial tachycardias | 12.28x |
| paroxysmal supraventricular tachycardias | 5.26x |
| bradyarrhythmias | 3.36x |
20231006 This paper from Korea yet again found that rates of various conditions were higher after COVID-19 than before:
- 12% higher risk of alopecia areata (spot baldness);
- 74% higher risk of alopecia totalis (losing all the hair on the head and face);
- 176% higher chance of antineutrophil cytoplasmic antibody-associated vasculitis;
- 68% higher chance of Crohn’s disease;
- 59% higher chance of sarcoidosis.
20231009 This paper from Canada found that people with immune-mediated inflammatory diseases (IMID) were 21% more likely to get a venous thromboembolism after getting COVID-19 than those without an IMID.
20230921 This paper from USA found that diabetes rose in young people. Here’s the number of diagnoses per 100,000 person-years pre- and post-pandemic:
| 2016-2019 | 2020-2021 | |
| Type 1 | 18.5 | 22.4 |
| Type 2 | 14.8 | 24.7 |
This paper from Singapore found that people who tested positive for COVID-19 had a 16% higher chance of having new-incident cardiovascular and cerebrovascular complications. The risk went down as the number of vax doses went up.


This paper from USA/Novavax provides some evidence for Novavax’s original formulation getting more durable the more shots you have. It’s a little hard to eyeball from the chart, but the correlates of protection dotted lines on the IgG antibody chart (top chart, A) imply that effectiveness drops from ~91% to ~76%(a 17% drop) in 154 days after the second shot, but only from ~95% to ~92% (a 4% drop) in 140 days after the third shot. (Yes, yes, 140 is smaller than 154, but I really don’t think the effectiveness is going to drop that much in two weeks!)

From the neutralization titres chart (bottom chart, B), it’s even more extreme. Eyeballing, the imputed VE drops from ~87% to ~50%? (wild guess, as the dotted lines don’t go that low) (a 43% drop) in 154 days after the second shot, but only from ~93% to ~87% (a 7% drop) in 140 days after the third shot.
And look at how strong three doses of the COVID Classic-based Novavax is against BA.4/5! I have been saying for a long time that my interpretation/extrapolation of what I’d seen was that Novavax gave weaker protection than mRNAs against variants the vaccine was based on, but that it gave broader protection. I’m glad to see data that pretty explicitly supports that.
This paper from Moderna says they made a version of its vax which doesn’t encode the whole spike protein, just two important parts which act as “keys” to “unlock” the target host cell. This new vax is fridge-stable instead of needing ultra-cold Even more importantly, it works as well or better (in mice) than Moderna Classic.
This makes sense to me: when presented with the whole spike protein, the human body could spend a lot of effort making antibodies that glom onto parts of the spike protein that don’t matter. If your immune system only sees the “keys”, it will only make antibodies that gum up the keys. More efficient! (Which maybe also means lower doses, which ought to mean lower side effects.)
This paper says that sub-lingual (non-injected) vaccines given to monkeys did a good job of eliciting IgA antibodies — the ones responsible for protecting mucous membranes.
(The paper made me imagine the poor scientists trying to put pills or liquids under the tongues of monkeys. Yeah, sublingual vaccination might be easier for humans, but I imagine that’s got to be one of the hardest ways to vaccinate monkeys!)
From a slide deck from the 12 Sept 2023 US CDC Advisory Committee on Immunization Practices meeting:

This preprint from South Africa and the UK says that the majority of Long COVID patients treated a with a combination of three different anti-coagulants had their symptoms resolve!
This paper from USA found that children who got two doses of vax were 46% less likely to test positive for COVID-19 if they showed up at the ER or to Urgent Care. The vaccine effectiveness was 30% against ER/Urgent Care visits and 40% against hospitalization.
That sounds pretty low, but the control — unvaccinated children — probably had a lot of COVID-19 infections.
COVID-Related Excess Death and Sickness
DEVON 202203 This paper from USA found that people who had COVID-19 infections had higher risks for various things than controls:
- 7.55x risk of respiratory failure;
- 5.66x risk of fatigue;
- 4.43x risk of hypertension
- 2.63x risk of memory difficulties;
- 2.59x risk of kidney injury;
- 2.50x risk of mental health diagnoses;
- 1.47x risk of hypercoagulability;
- 2.19x risk of cardiac rhythm disorders.
Note though, that compared to a historical pre-COVID group which had viral lower respiratory illness, only respiratory failure, dementia, and post-viral fatigue had increased risks! Viruses are just plain nasty, don’t catch them!
20230906 This preprint from UK says that people who got vaccinated then got a COVID-19 infection had higher levels of anti-spike antibodies, but lower levels of anti-nucleotide antibodies than unvaccinated people who got infected. They theorize that maybe being vaccinated meant that they didn’t get as sick, so didn’t create as strong a reaction to the nucleotide proteins. (Reminder: the vaccines don’t have nucleotide proteins.)
They also found that higher levels of anti-spike antibodies correlated with shorter duration infections, though the severity of the symptoms seemed to be about the same. However, people with higher anti-spike antibodies were less likely to have six or more symptoms and also had lower Ct values (which correlates with infectiousness, I believe).
20230821 This paper from USA found that the all-cause mortality for COVID-infected veterans between March 2020 and April 2021 was six times that of non-infected veterans in the first three months of infection. It was ~20% higher in months 3-6, and actually slightly lower from six months to two years. This is probably due to the most vulnerable dying earlier than they would have without COVID-19.
20230907 Some good news! This paper from Netherlands found that in a group of elite athletes, 3% had MRIs which suggested myopathy (muscle fibres not functioning properly), but all of them returned to elite-level competition within 26 months. None of the athletes had to drop out of elite-level competition due to COVID.
DEVON 20230821 Aaand back to bad news: this paper from USA found that people who had COVID-19 were more likely than uninfected controls to develop high blood pressure which was persistent for at least six months. People who had not been hospitalized were 52% more likely to get high blood pressure than controls; people who had been hospitalized were 2.23 times as likely to get hypertension.
202305 This report from the US Society of Actuaries found that the 2021 non-COVID deaths were ~15% higher than the baseline (pre-COVID) deaths. In 2022, non-COVID deaths were ~12% higher than baseline deaths. This might be undercounting of COVID deaths, or it might be that COVID-19 is hard on the body and damages it in ways that don’t show up immediately.
DEVON 20230721 This paper from UK found that for at least two years after COVID-19 infection, adults scored on cognitive tests like they were ten years older. The paper did say they only found effects in people who reported that they did not feel fully recovered, but that might be because people who had cognitive difficulties could tell that their brains weren’t working right.
DEVON 20230816 This paper from Hong Kong found that COVID-19 put you at elevated risk for many illnesses, with adjusted hazard ratios of:
- multiple sclerosis: 2.66x;
- pernicious anemia: 1.72x;
- spondyloarthritis: 1.32x;
- rheumatoid arthritis: 1.29x;
- other autoimmune arthritis: 1.43x;
- psoriasis: 1.42x;
- pemphigoid (a skin disease): 2.39x;
- Graves’ disease: 1.30x;
- anti-phospholipid antibody syndrome 2.12x;
- immune mediated thrombocytopenia: 2.1x;
- vasculitis: 1.46x.
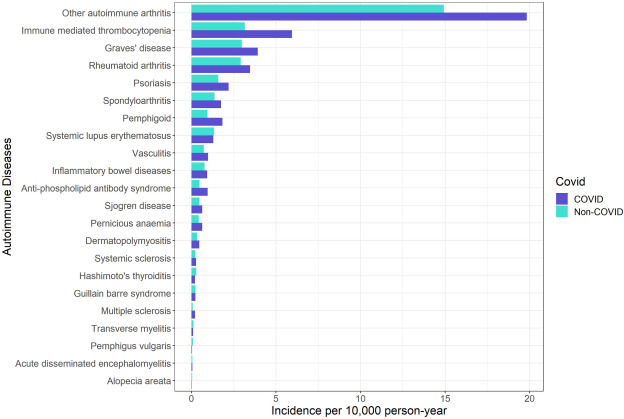
They also said that vaccination reduced the risk for most of the above ailments.
DEVON
20230511 This paper using data from Hong Kong and the UK calculated the increased risk of various things after the acute phase of COVID-19 ended for 17 to 28 months. They found:
- 1.82x risk of heart failure;
- 1.31x risk of atrial fibrillation;
- 1.32x risk of coronary artery disease;
- 1.74x risk of deep vein thrombosis;
- 1.61x risk of chronic pulmonary disease;
- 1.89x risk of acute respiratory distress syndrome;
- 3.91x risk of interstitial lung disease;
- 2.32x risk of seizure;
- 1.65x risk of anxiety disorder;
- 1.52x risk of PTSD;
- 1.76x risk of end-stage renal disease;
- 2.14x risk of acute kidney injury;
- 1.42x risk of pancreatitis;
- 2.86x risk of cardiovascular mortality;
- 4.16x risk of all-cause cardiovascular mortality. (I.e. you are four times as likely to have a cardiovascular issue which kills you in the ~2 years after you have COVID-19.)
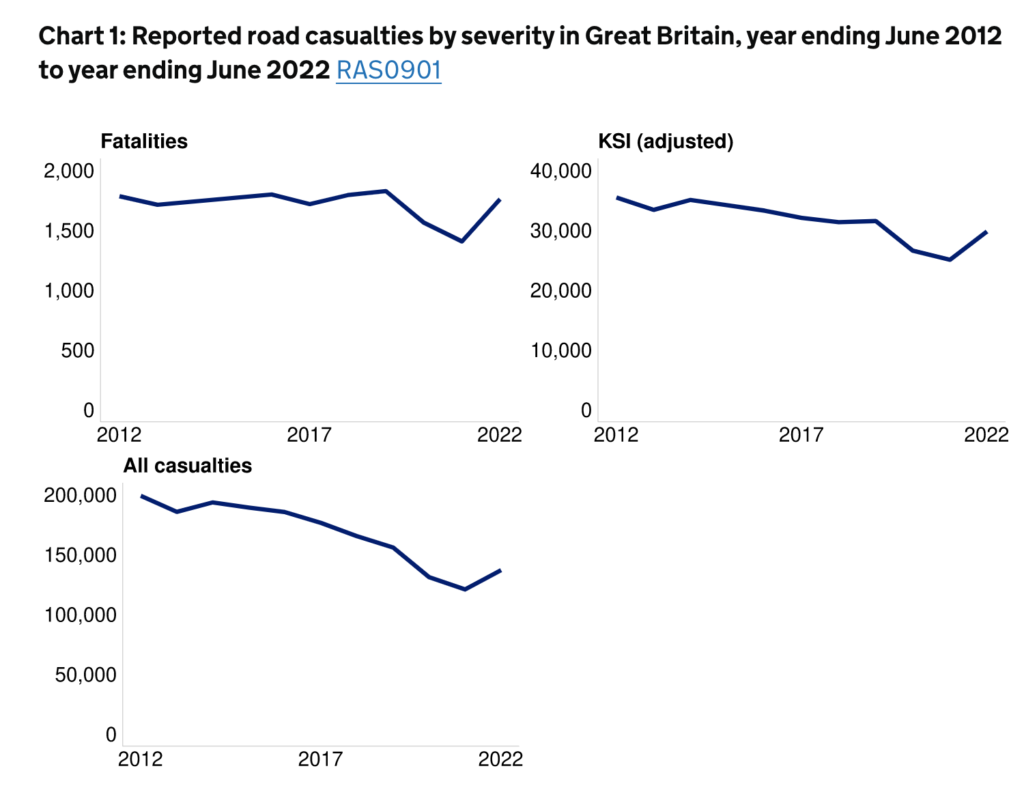
DEVON Traffic accidents
20230614 In this paper from Brazil, they found that a quarter of people who had had mild COVID-19 infections (mostly mild) had unusual difficulty in using visual and spatial information to guide complex behaviors (like drawing, assembling objects or organizing multiple pieces of a more sophisticated stimuli).
I am not the only person who wonders if this could be related to the increase in traffic accidents since the pandemic started. This is not the first paper to connect COVID-19 with accidents: See for example:
This paper from Canada from Feb 2023 finding that unvaccinated people were 48% more likely to get in traffic accidents than vaccinated people (after adjusting for age, sex, home location, socioeconomic status, and medical diagnoses).

This report from the US National Highway Traffic Safety Administration found that traffic fatalities increased hugely post-lockdowns over pre-pandemic levels.

This article from France from now reports that while the total number of accidents in 2021 was about the same as pre-pandemic, there were big jumps in the number of motorway fatalities (up by 12% over pre-pandemic) and cyclist deaths (up 30%).
This article reports that traffic fatalities in 2022 were up at least 10% over 2019 in the Netherlands.
However, this report from the UK government from Nov 2022 says that traffic accidents were down in the UK compared to pre-pandemic.
This paper from USA found that people who had had COVID-19 infections were about three times as likely to have a low ratio of stress myocardial blood flow to resting blood flow. Yeah, okay, that’s a kind of strange measure, but basically it means they can’t boost their blood flow as much when they need it.
20230522 This paper from Germany finds (yet again) that COVID-19 infections lead to a higher risk of coming down with diabetes. They found that the risk of Type 1 diabetes was 57% higher in children who had had COVID-19 infections.
20230519 This article reports that the number of people diagnosed with atrial fibrilation has increased by 50% in the past ten years.
20230515 This paper from Brazil found that COVID-19 can take up residence in the liver, where it induces high blood sugar (which is probably why the diabetes risk goes up after a COVID-19 infection).
20230420 This preprint from Scandinavia found that people who were bedridden (note, not necessarily hospitalized!) for at least seven days with COVID-19 had a 125% higher prevalence of severe physical symptom burden (scores higher than 15 on PHQ-15, the Patient Health Questionnaire) over the course of 27 months. People who had COVID-19 but were bedridden for less than seven days didn’t have any more severe physical symptom burden than controls.
This paper from Austria from April 2021 and this paper from the USA from May 2022 both found that patients who had had COVID-19 infections were significantly likely to have REM sleep without atonia (the muscles going completely relaxed). This international paper from April 2022 found that people who had had COVID-19 infections were about three times more likely to have deam-enactment behaviours (which means making physical motions during the dream, which necessarily means they also didn’t have atonia).
Meanwhile, 20150317 this paper says that 80% of people who have REM without atonia go on to develop Parkinson’s. Ulp.
This preprint from UK from October 2022 found that people who had had COVID-19 infections were 22% more likely to get immune mediated inflammatory diseases than the non-infected. In particular, people who’d had COVID-19 were:
- 56% more likely to get type 1 diabetes;
- 52% more likely to get inflammatory bowel disease;
- 23% more likely to get psoriasis.
20230308 This paper from Croatia found that arterial walls get stiffer after a COVID-19 infection, even a mild case. Worse, they found that over the 3-month length of the study, arterial walls continued to get stiffer instead of getting better. They hypothesize that the stiffening is because of chronic inflammation.
DEVON DEVON DEVON 20230110 This paper from Taiwan using US data found that the risks of autoimmune disorders was way way higher in the six months after getting COVID:
| Disease | Adjusted Hazard Ratio |
| rheumatoid arthritis | 2.98 |
| ankylosing spondylitis | 3.21 |
| systemic lupus erythematosus | 2.99 |
| dermatopolymyositis | 1.96 |
| systemic sclerosis | 2.58 |
| Sjögren’s syndrome | 2.62 |
| mixed connective tissue disease | 3.14 |
| Behçet’s disease | 2.32 |
| polymyalgia rheumatica | 2.90 |
| vasculitis | 1.96 |
| psoriasis | 2.91 |
| inflammatory bowel disease | 1.78 |
| celiac disease | 2.68 |
| type 1 diabetes mellitus | 2.68 |
| death | 1.20 |
20230418 This paper from UBC (go UBC!) found that people in BC who tested positive COVID-19 tests in the first two years of the pandemic were 17% more likely to get diabetes than people who had not. For males, it was even worse — a 22% higher risk. This meant about 3.4% of the new diabetes cases in BC resulted from COVID-19 (4.75% for males).

The risks got higher as the COVID-19 infections got worse: 142% higher risk for those hospitalized and 229% higher risk for those admitted to the ICU.
DEVON 20230418 This blog post talks about the UBC paper and another TWELVE studies which also found increased risk of diabetes after COVID-19 infections, plus talked about possible mechanisms.
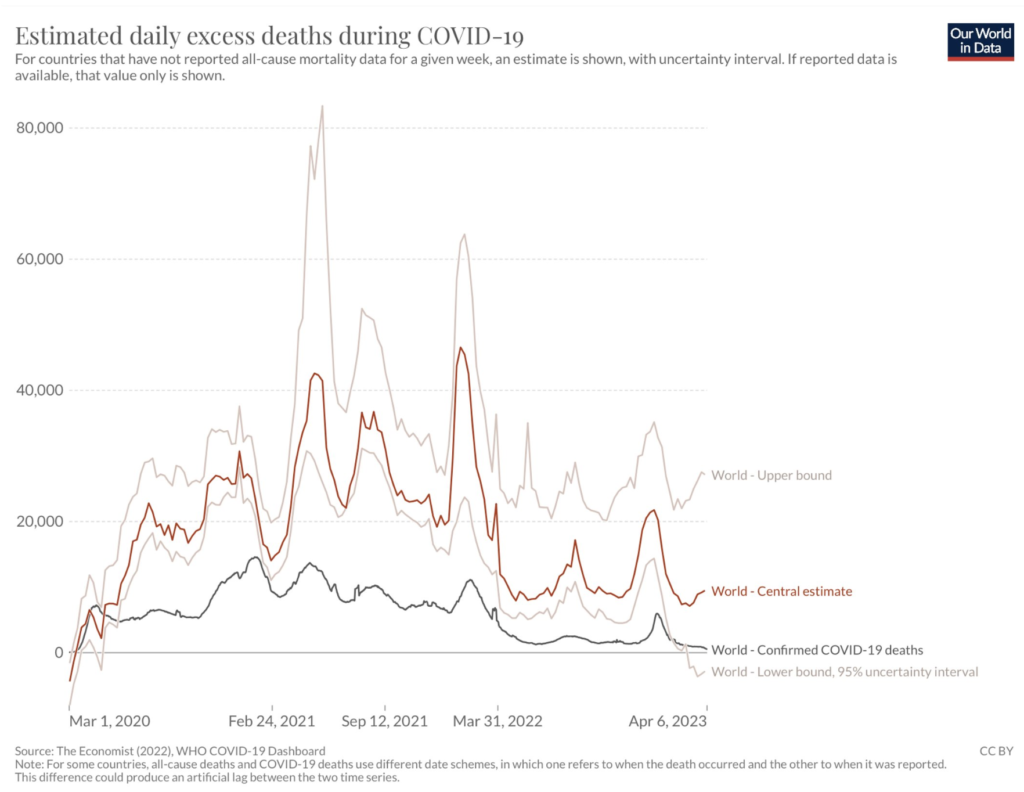
As per 20230411 this tweet (referring to the graph below), the global COVID-19 death rate is going down, but the excess deaths are going up. How can this be? It’s a sign that COVID-19 causes long-term damage to the human body, which manifests itself in early deaths that don’t look like COVID-19.
This paper from the US found that hospitalized COVID-19 patients were much more likely to get secondary infections in the hospital (e.g. catheter-associated urinary tract infection) than non-COVID-19 patients. They don’t know if it’s just from the longer hospitalization stay (8.2 days for COVID-19 patients vs. 4.7 days for non-COVID patients), maybe it’s due to COVID-19 wards being more frantic, or if it is from something about COVID-19 itself.
20230323 This paper from USA found that baby boys born to mothers who had COVID-19 infections during pregnancy had twice the risk of a diagnosis of a neurodevelopmental issue than mothers who did not have COVID-19. Baby girls were not affected.
20230415 This paper from UK found that 62% of people who had been hospitalized with COVID-19 had sleep disturbances after they got out, and that having sleep disturbances correlated with having impaired lung functioning. Yeah, I also can’t sleep well when I can’t breathe well (from a stuffed up nose). (Oddly, the study authors framed it the other way around, as if trouble sleeping caused trouble breathing.)
202304 This study of pediatric diabetes in Finland in the first seventeen months of the pandemic found that kids were diagnosed with type 1 diabetes at a rate of 61 per 100,000 compared to 52.3 per 100,000 before the pandemic. The pandemic kids were also sicker when diagnosed compared to the pre-pandemic kids. However, only 0.9% of the pandemic-diagnosed kids had COVID-19 antibodies! That’s bizarre. Maybe having schools closed meant they got less exercise?
DEVON DEVON 20230303 This paper says that people who had COVID-19 were at much higher risk in the year after their infection for a variety of things than people who never had COVID-19:
- 2.35x risk of cardiac arrhythmias;
- 3.64x risk of pulmonary embolism;
- 1.78x risk of coronary artery disease;
- 1.97x risk of heart failure;
- 1.94x risk of chronic obstructive pulmonary disease;
- 1.95x risk of asthma.
In addition, people who had COVID-19 infections were 1.5 times as likely to die in the year following infection.

20230307 This paper from the USA found that people who had COVID-19 infections were at a higher risk over the course of the next year for a ton of different gastrointestinal issues than people who never had COVID-19. Very broadly speaking, the risks were generally sort of between 1.5x and 2x, and the risk was higher the worse their original infection was.
20230214 This paper from USA is yet another which says that people are more likely to develop diabetes after a COVID-19 infection than the uninfected. In this paper, they found an adjusted increased risk of 58%.
20230126 This preprint from Germany found that people who got COVID-19 infections were at a 43% higher risk of developing an auto-immune disease. The list of autoimmune diseases that they were at higher risk for was very long, and included Hashimoto’s disease, diabetes, MS, Behcet’s disease, scaroidosis, Wegener’s disease, and vitiligo.
20230126 This is worrying. This preprint from France found that the risks in children of acute tubulointerstitial nephritis (kidney infection) was higher after a COVID-19 infection. The absolute numbers were low — only 41 kids in all of France — but the relative risk was very high. The risk of acute tubulointerstitial nephritis without uveitis was 3x higher and the risk of acute tubulointerstitial nephritis with uveitis was 12x higher. This is just more proof that COVID-19 f’s with the whole body.
DUPLICATE 20230110 This paper from Taiwan says that getting a COVID-19 infection gives a higher risk of a long list of auto-immune disorders. Over two years, the risk of getting these things for people who had a COVID-19 infection vs. those who had not gotten infected was:
- rheumatoid arthritis: 2.98x;
- ankylosing spondylitis: 3.21x;
- systemic lupus erythematosus:2.99x;
- dermatopolymyositis:1.96x;
- systemic sclerosis: 2.58x;
- Sjögren’s syndrome: 2.62x;
- mixed connective tissue disease: 3.14x;
- Behçet’s disease: 2.32x;
- polymyalgia rheumatica: 2.90x;
- vasculitis: 1.96x;
- psoriasis: 2.91x;
- inflammatory bowel disease: 1.78x;
- celiac disease: 2.68x;
- type 1 diabetes mellitus: 2.68x.
This is all on top of a 1.2x risk of death.
20220715 This paper from Denmark says that the risk of developing a neurological disorder is about doubled after COVID-19. However, they note that this doesn’t seem to be any higher than after similarly severe infections.
