NB: I hurt a tendon in my hand, so took a few days off from typing. It will probably take me a few days to catch up on all that has happened.
Treatments
A big study in the UK found that giving people in hospital convalescent plasma (i.e. a source of antibodies) did absolutely no good. STUNNINGLY no good. It was, in fact, really surprising that it helped so little. Giving antibodies ought to be useful, right???
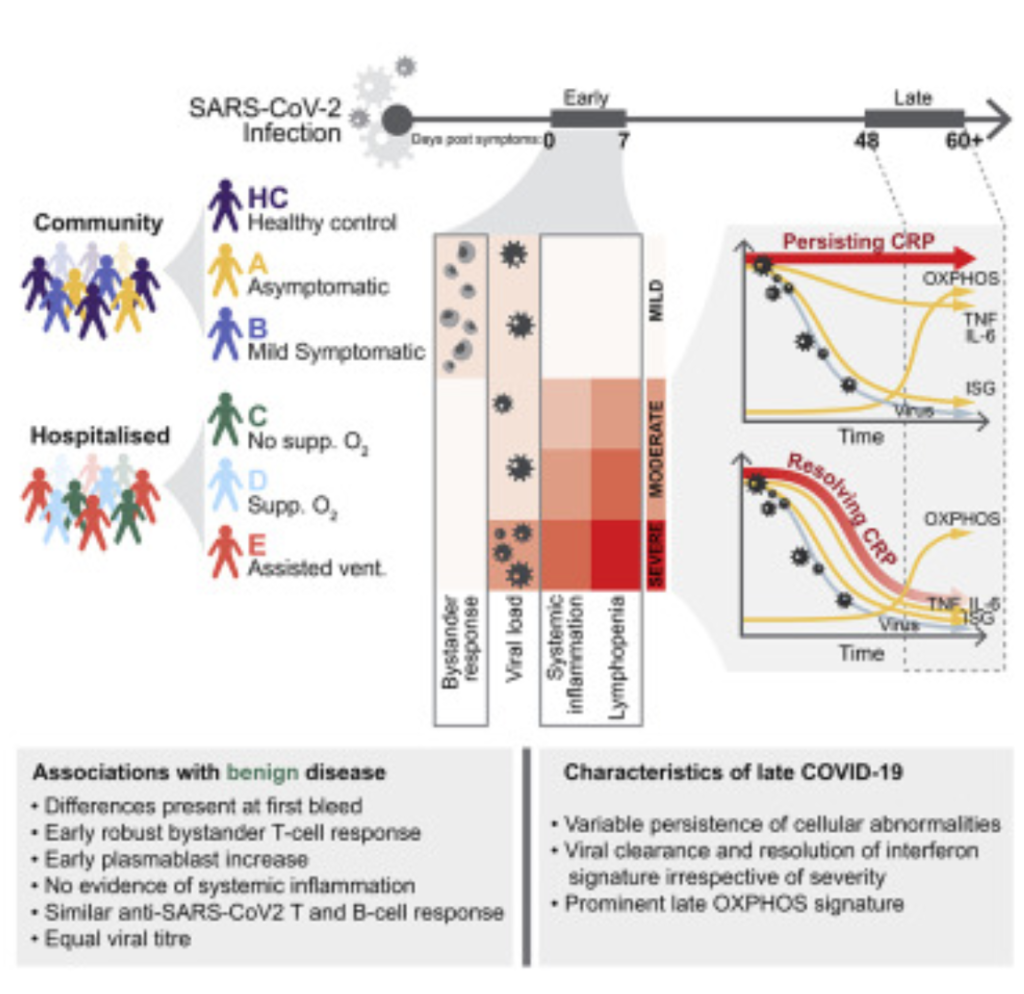
WELL. It turns out that it’s all about the Ts, ’bout the Ts, no antibodies. This paper says found a clear difference between mild and severe cases that was mostly in the bystander T cell response.
Okay, you’re asking. “What’s a bystander T cell?” Um, it turns out that the immune system is insanely complicated. (Trying to figure it out is like trying to figure out uncommented assembly code written by noobs who use lots of JMPs!) It is so complicated that I am not going to be able to explain it all, and what I do explain is likely to be an egregious simplification at best and wrong at worst. But here goes:
Normally, helper T cells (whose job it is to raise an alarm) need to bump into an antigen (bad guy) before raising the alarm. Normally, they need to bump into a specific bad guy before raising the alarm, so really it’s more like they yell, “JEFFREY EPSTEIN! JEFFREY EPSTEIN! HELP HELP HELP!!!” Sometimes, however, T cells who are trained to recognize someone else (say, Idi Amin) who happen to be in the neighbourhood (i.e. are bystanding) get recruited to help yell, in which case they just yell “HELP HELP HELP!”. This causes players in the non-specific immune system (called interleukins) to come rushing over to help out.
(Any immunologists out there want to correct me? I’ll post any corrections.)
But the bottom line is that by the time they get to the hospital, COVID patients have antibodies, but that’s not sufficient. By the time they get to the hospital, it’s too late, their viral load is too high, they have real trouble killing all the virus. (I think that’s why patients get a cytokine storm — the immune system is throwing everything they’ve got at the virus.) In mild cases, however, the early bystander T cells are able to marshal enough forces to the battle that the viral load doesn’t get out of control before the B cells and killer Ts can arrive on the scene.
I just said that antibodies didn’t matter, that it was the T-cells? Well, this paper says that high levels of antibodies correlate highly with the efficacy of a vaccine. This is important because it is much easier to test the blood of someone who has was vaccinated two weeks before, than to vaccinate a half a gazillion people with a vax, half a gazillion people with a placebo, and wait weeks and weeks for enough people to get sick out of the gazillion people to be able to tell what the efficacy of the vax is.
This is particularly important for boosters. Suppose there is some nasty new scariant which pops up. If the vax makers can convince the regulators that you only need to look at the antibody levels and not a full-blown random controlled trial, then they could conceivably get approval in around three months.

This article talks about a new antiviral small-interfering RNA to directly attack COVID-19.
Vaccines
The EMA, the European regulatory agency, changed the storage requirements for the Pfizer/BNT vax to allow storing in a normal fridge for a month! Awesome!
A scientist in Germany thinks he can explain why AZ (and maybe J&J) sometimes form blood clots.
There’s two important ingredients in the AZ vax:
- fragments of human cells from the cell line which is used to grow the adenovirus which the AZ and J&J vax depend upon to get their payloads into the patient’s cells
- a preservative called ethylenediaminetetraacetic acid (ETDA) which is known to sometimes make blood vessels leaky
The ETDA, by making the blood vessels leaky, could allow the vaccine to escape out of the lymphatic system into the blood system. In the blood system, it could then encounter platelet factor 4, which platelets secrete.
The scientist says he saw (in the lab) platelet factor 4 grab some human proteins from the vaccine, and form a big glob. He theorizes that
- this glob is big enough that the immune system notices it;
- the immune system (which is already hyper-excited, having gotten revved up by the vaccine) decides the glob is a threat;
- the immune system makes antibodies to the glob, including platelet factor 4;
- without platelet factor 4, clotting goes way up.
ETDA is not listed specifically in the J&J ingredients, but it might be one of those things where they just say “preservatives” in the same way that food ingredient lists will just say “spices” (which is of zero use to anyone who is allergic to e.g. garlic or turmeric).
This article says that delaying second doses and mixing&matching probably are/were good ideas.
There was a study in the UK which says that delaying the second dose gives a better result: 3.5x more antibodies in older folks.
Sanofi/GSK is about to start Phase 3 trials of two vaccines. One is based on COVID Classic, one is based on B.1.351. I mention this for a few reasons: Canada has contracts for 52-72M doses, Sanofi has a plant in Quebec, so it’s possible that the vax could be manufactured here; Sanofi and GSK both have lots of practice with vaccines and could credibly make 1B doses this year.
Hilda Bastian is an absolutely phenomenal resource on vaccines. She occasionally writes up everything she knows, so if you want a LOT of information on the different vaccines, see her most recent encyclopedia. Here’s a nice graphic that summarizes a piece of it:

The vaccines are very likely to be able to hold up against the e B.1.617 and B.1.618 variants.
