Variant of Concerns
Californa
There is a strain in California which appears to be more contagious, the B.1.427/B.1.429 strain, which has a single interesting mutation (L452R). It is not in a specific part of the spike protein called the Receptor-Binding Domain (RBD).
According to the un-peer-reviewed information, the variant appears to be more contagious: people with that strain have a higher viral load in their nostrils. It might be more deadly, (although that sample size is small). Vaccines are somewhat less effective against it in vitro, they aren’t sure yet of how it will react in vivo; the researcher quoted in all these articles thinks it won’t be as resistant as B.1.351 (the South African variant).
This is very early news: the research papers aren’t even in the preprint stage; I’ve had trouble finding hard information on it. It seems like the news articles just relied on interviews with the scientists. So take it with a grain of salt.
See
- A California Department of Public Health report which alerts that the strain exists
- A preprint talking about the genetics of the strain
- an LA Times article: “Over five months starting on Sept. 1, the California strain […] rose from complete obscurity to account for more than 50% of all coronavirus samples that were subjected to genetic analysis in the state.”
- a New York Times article on the spread
- a New York Times piece of an article on the mutation
- an article in Science
South Africa B.1.351
A Cell preprint shows that antibodies to COVID-19 in people vaccinated or infected with COVID Classic aren’t able to get rid of B.1.351 in vitro. (NB: The body generally does better at killing viruses than these in vitro trials because in vitro only tests one (very important!) piece of the immune system while the human immune system has lots of different pieces.)
A different Cell preprint also found that B.1.351 has antibody escape, but that it was not more infectious. So it’s not easier to catch, but if you had a different strain of COVID, that won’t protect you.
COVs and antibodies
There is some nice research discussed in this thread about which mutations cause which specific antibodies to become ineffective. They looked at the two antibodies which are used in the Regeneron antibody cocktail, LY-CoV016 and LY-CoV555:
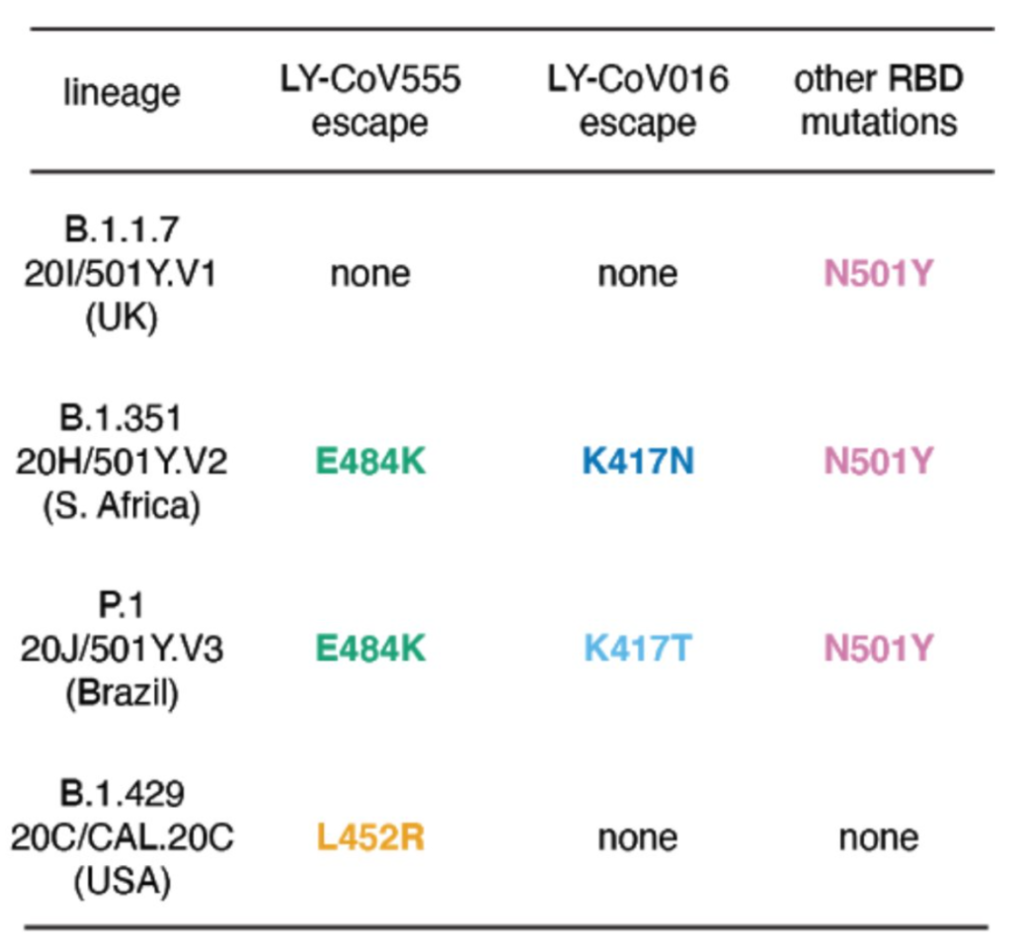
Translation: the Regeneron cocktail will work fine against B.1.1.7, will probably have reduced effectiveness against B.1.429, and won’t work at all against B.1.351 and P.1.
Superspreading
Over and over again, superspreader events have been shown to happen in the same kinds of spaces: crowded indoor spaces with poor ventilation, especially where yelling or singing is taking place.
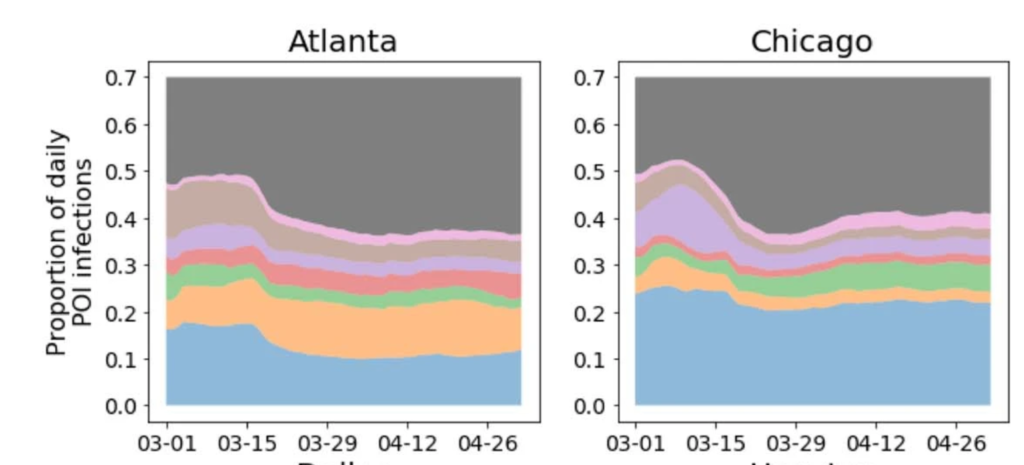
Today there were two very good Nature articles, one technical and scientific and a broader one which said the same basic thing but targeted more for a mass audience and included further information: The researchers studied mobility data and combined it with information about the businesses where people went.
From the more technical paper:
- The majority of superspreader events occurred at a minority of the locations, which implies that restricting the maximum occupancy at dangerous locations is more effective than uniformly reducing mobility.
- You can achieve a disproportionately large reduction in infections with a small reduction in visits.
- A large reduction in occupancy percentage results in a smaller reduction in visits. For example, they modelled that an 20% occupancy restriction, which you would think would lead to an 80% reduction in visits, in fact only resulted in a 42% reduction in visits.
- Full-service restaurants, gyms, hotels, cafes, religious organizations and limited-service restaurants produced the largest predicted increases in infections when reopened.
- Certain types of locations (e.g. full-service restaurants and hotels) had a disproportionally large share of infections. (See the paper’s Figure 2, parts of which are reproduced below.)
- Disadvantaged people have not been able to reduce their mobility as sharply, and that places they visit are more crowded and thus with higher risk; this can help explain why disadvantaged people have gotten COVID at higher rates.
- The magnitude of mobility reduction is at least as important as its timing.

From the more mass-audience article:
- Singing, shouting, aerobic exercise, and even just talking loudly produce more aerosols than not talking or speaking quietly: “Estimates suggest that speaking loudly can increase the number of particles emitted by up to 50 times compared with normal speaking, and singing can produce up to 99 times more, according to a study that has not been peer reviewed.”
- Some individuals naturally speak louder or expel more air when they exhale, so they presumably emit more aerosols. Women and children probably emit fewer because of a smaller lung capacity.
- There are “super-emitters”; 20% of the people emit 80% of the particles. People who are older or overweight produce more aerosols than others.
- Superspreaders usually were asymptomatic or only had mild symptoms.
- They found a lower dispersion parameter (meaning “clumpier” distribution, a higher percentage of infections coming from superspreaders) among people under 60 and in rural areas.
- Cluster-focused backwards contact tracing — following the transmission chain back in time to locate the individual who infected the person in question — has an oversized effect on controlling transmission. (Unfortunately, it’s expensive enough to do that it’s only really practical when you have a relatively small number of cases.)
A Medarxiv paper suggests that viral loads relevant to infection from presymptomatic or mildly symptomatic individuals may fall into a narrow range, and that exceptionally high viral loads are not required to induce a superspreading event. In other words, it’s the behaviour, not the person.
A paper in Nature on the sources of variation in particles emitted finds:
- Even quiet speech yields significantly more particles than normal breathing.
- The louder you talk, the more particles you emit, regardless of the language spoken (English, Spanish, Mandarin, or Arabic).
- A small fraction of individuals behaves as “speech superemitters,” consistently releasing an order of magnitude more particles than their peers.
A Journal of Aerosol Science article found that:
- Breathing through the mouth produced about twice as many particles as breathing through the nose.
- Whispering produced only slightly more particles than breathing through the mouth.
- Speaking normally produced a bit more than twice as many particles as whispering.
- Going “aaaaaah” produced almost ten times more particles than breathing through the mouth.
Eyes
This article in The Lancet says that eyes are an unacknowledged weak spot in the human defenses against COVID-19.
- It cites another study: “A large study showed that 19% of health-care workers became infected, despite wearing three-layered surgical masks, gloves, and shoe covers and using alcohol rub. After the introduction of face shields, no worker was infected”.
- It points out that the exposed area of the eyeballs is much bigger than the exposed area of the nose or mouth.
- It explains how COVID-19 could theoretically enter via the eyes.