COVID-19
COVID-Related Excess Death and Sickness
There have been a fair number of articles and post on teh socials wringing hands about how cancer rates in young people were risking — with the implication that it was because of COVID-19 infections or vaccines. However, the data for that hand-wringing had been pre-pancemic.
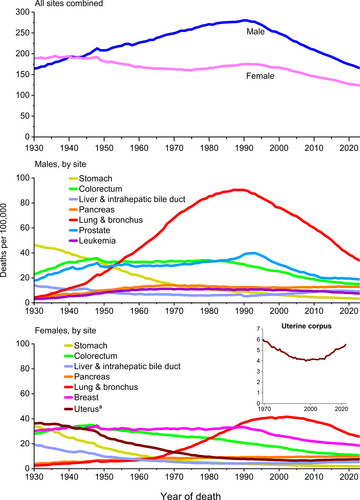
Good news! We just got an update. This report from USA (2026-01-13) doesn’t give breakouts by age over time, but does go through 2022 for incidence and 2023 for mortality. I do not see any indication from their graphs that COVID-19 had any effect on cancer mortality in the USA:
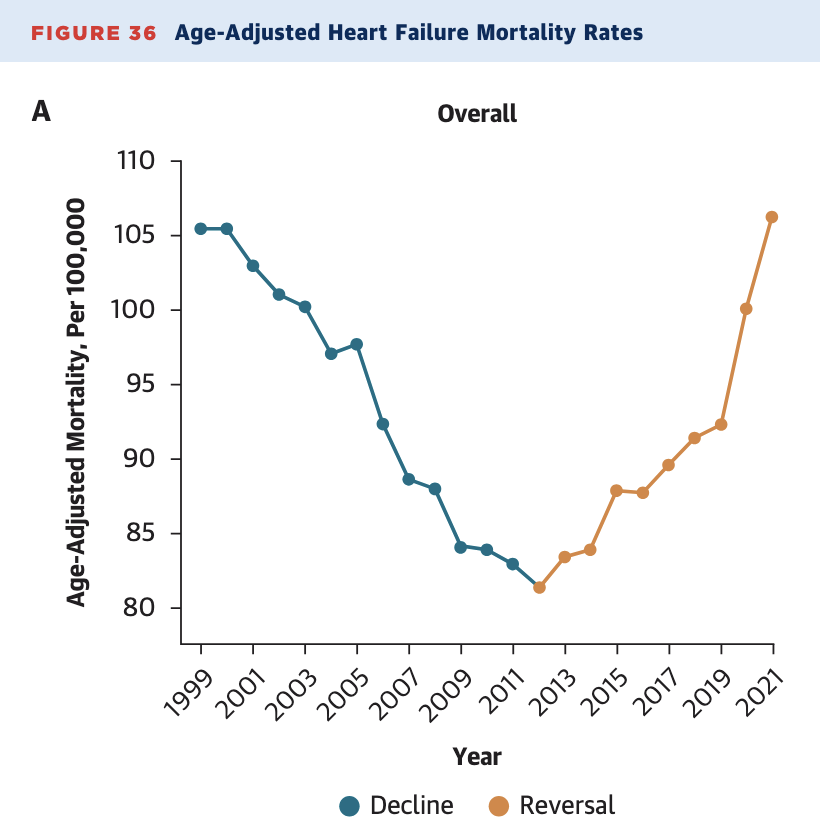
This paper from USA (2026-01-12) reports that while the rate of heart failure has been going up since 2012, it really went up in 2020/2021. This article about the paper (2026-01-12) points out that heart failure reflects cumulative damage.
💊🎉🐁 This paper (2026-01-07) reports on mice who were infected with a mouse-adapted version of SARS-CoV-2 and developed something that looked a lot like neurological Long COVID, with smell and cognitive disorders. Mice who were given Paxlovid were partially protected from neurological damage, but mice who were given Paxlovid and corticosteroids were completely protected from smell/cognitive disorders!
💉 This paper from Portugal (2025-11-07) reports that people who were hospitalized for COVID-19 but did not get a COVID-19 vaccination had about twice the risk of a “cardiovascular event” at least 30 days after infection, compared people who did get a vax.
🩸 This paper from USA (2025-01-22) reports that the risk of a thrombotic event (i.e. blod clot messing something up) was higher among COVID-19 patients than patients with other respiratory illnessess:
- for hospitalized patients, the ones who had COVID-19 had a 63% higher risk of a thrombotic event in following year than people who had a different respiratory disease;
- for patients who sought medical treatment but were not hospitalized, the ones who had COVID-19 had a 73% higher risk of a thrombotic event in following year than people who had a different respiratory disease.
I couldn’t tell if the hospitalized patients had to be hospitalized for a respiratory disease or if they counted anybody with a respiratory disease.
Long COVID
😬🩸🧠 This paper from USA (2026-01-05) reports that people with Long COVID had elevated levels in the blood of some of the proteins you usually see with Alzheimer’s Disease.
It can be difficult to figure out what the risk of “bad Long COVID”, (where your life is totally upended) is, since just about any long-term symptoms are rightfully called Long COVID. Well, this unedited manuscript from Germany (2025-12-30) found that 1.1% of the people (in a sample of about 5000 people) who had PCR-tested positive for COVID-19 were continuously on sick leave since their initial SARS-CoV-2 infection to the end of the study (about 24 months).
Mitigation Measures
🧽🫧 This older paper from USA (2022-04-04) found that enhanced cleaning at 17 schools gave about a 20% reduction in absences due to gastrointestinal illnesses, but it had no effect on absences from respiratory illnesses. This aligns with other research I’ve seen that says that surface transmission (fomites) is not a major spreader of COVID-19 or influenza. (NB: The last doctor I talked to — who seemed quite current on many things — thinks that influenza does spread a fair amount via surfaces, so maybe I am wrong.)
This paper from USA (2026-01-13) found that people with a family history of cancer were 26% more likely than controls to get Long COVID. This dropped to 16% when “health conditions were accounted for”.
Transmission
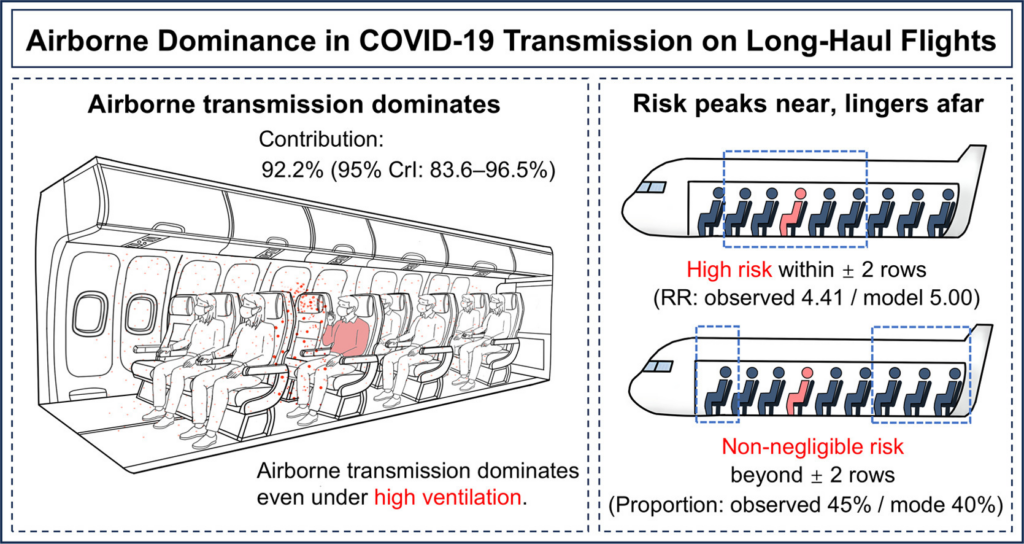
✈️ This paper (2026-01-09) concluded that even on airplanes — where there is pretty high airflow and HEPA filters — the dominant transmission mode is via airborne transmission (i.e. aerosols). 92.2% of transmission was airborne, with only contact (i.e. fomites) only accounting for 7.8% of transmission. Direct deposition (i.e. large droplets) accounted for zero of the transmissions.
They also found that the risk was a lot higher for people who were sitting within two rows of a contagious person — 4.41 times higher risk — compared with those farther away.
Note that this study was a close look at one flight, but from what I can tell, they didn’t consider (at all) boarding and disembarking from the plane (where the ventilation and filters are completely off). We don’t know how many people got infected when they were putting their baggage away and how many got infected during the flight.
🦠 This paper from USA (2025-04-29) reports that antimicrobial-resistant infections went up a lot during the peak of the COVID-19 pandemic. Infections classified as in-hospital infections went up by 31.5% over the pre-pandemic baseline and infections classified as out-of-hospital went up by 6.5%. The hospital-acquired infections appear to be because of there being much more traffic of sicker patients.
After the peak of the hospital crush, the rates dropped. Out-of-hospital infections dropped to baseline, but in-hospital infections were still 11% over the pre-pandemic baseline.
Pathology
This preprint from USA (2026-01-02) reports that after a COVID-19 infection, patient have reduced mitochondrial function in T cells. (Translation: COVID-19 fucks with a very important piece of the immune system that recognizes viruses you’ve seen before.)
This paper from Spain (2026-01-13) reports that the COVID-19 hospitalization fatality rate is 13.7% overall, and 24% for people over 79 years old. (In other words, for 1000 people hospitalized for COVID-19, 137 come out in a bag.)
Comorbidities played a strong part. Compared to people without comorbidities, the following raised the risk of death in patients hospitalized for COVID-19:
- solid tumours: 6.25 times higher risk;
- blood malignancies: 7.98 times higher risk;
- diabetes: 4.81 times higher risk;
- high blood pressure: 4.22 times higher risk.
🐈⬛ Cyprus had a huuuuuge outbreak of FCoV-23, a feline coronavirus in 2023. This article (2025-12-25) says FCoV-23 turned out to be a novel recombination of a cat coronavirus and pCCoV, a dog coronavirus!.
A bad immune response to feline coronaviruses causes feline infectious peritonitis (FIP), which is almost always fatal, and FCoV-23 seemed to almost always cause FIP. 😬 Fortunately, this paper (2018-05-05) showed that human treatments for COVID-19 (especially remdesivir and a metabolite of remdesivir called GS-441524) could treat feline coronaviruses with a high save rate, and leftover meds from treating COVID-19 in humans saved a lot of cats.
For a long time, they thought that FIP viruses only infected monocytes/macrophages, but this paper from USA (2026-01-06) reports that the feline coronaviruses infects T cells and B cells as well as monocytes and macrophages. 😬 This is bad, as those are kinda important players in the immune system. 😬😬 Worse, sometimes some of those infected cells hang around even after the symptoms of the acute disease went away. 😬😬😬 Worst, as a coronavirus, it’s easy to imagine this happening with COVID-19.
Vaccines
💉 HA! I have been questioning for years whether the studies that found that “more vaccines equals more better” were actually about “more recent vaccination equals more better”. This paper from Greece (2026-01-14) found that anti-COVID antibody levels were a function only of how long it had been since the last vaccination or infection, not the number of vaccines the participants had gotten.
💉 This paper from England (2026-01-12) looked at how many people were vax-hesitant, why, and if they overcame it. They found that hesitancy changed over time:
- Hesitancy peaked at 8.0% in early 2021;
- hesitancy decreased to a low of 1.1% at the start of 2022;
- hesitancy rose to 2.2% in early 2022.
65% of hesitant people eventually got one or more vaccinations.
They categorized eight reasons for hesitancy:
- Cluster A (the largest group) included concerns about vaccine effectiveness and general concerns about short-term and long-term side-effects;
- cluster B (a very small cluster) included concerns about travel to the vaccination centre;
- cluster C included perception of low risk from COVID-19 and mistrust of vaccine developers;
- cluster D included personal health concerns;
- cluster E (another big cluster) included fear of vaccines, previous adverse reactions, and generalised anti-vaccine sentiment;
- cluster F included fertility and perceived lack of need because of having had COVID-19 previously;
- cluster G included concerns over pregnancy or breastfeeding and the response “Prefer not to say”;
- cluster H included the response “Other” and concern over doses being limited.
People whose hesitancy related to effectiveness and health concerns mostly eventually got vaccinated. People who had low trust, who thought they weren’t much at risk from COVID-19, and who had a generally higher anti-vax sentiment tended to not get vaccinated.
💉 This paper from USA (2026-01-10) reports that Moderna’s vaccine for last year (the KP.2 version of Spikevax) was reasonably effective, with vaccine effectivenesses (VEs) of:
| against | within 55 days (median) | within 127 days (median) |
| hospitalization | 52.8% | 45.2% |
| any healthcare system attention | 39.4% | 33.1% |
Pandemic Side Effects
🕷️🩸🧪 Okay, this is the strangest side-effect of the pandemic that I’ve seen: shortages in Australian spider anti-venom. This article (2026-01-13) says that you need venom to make antivenom. You need to milk spiders to get venom. The spiders take a few years to mature to the point where they can be milked. The people who raise spiders depend upon private citizens to donate spiders and/or egg sacs that they find. One of the early pandemic’s mitigation measures in Australia was to restrict people from going more than two kilometers from their homes. That meant that donations of spiders and eggs dropped, which cascaded into there being a bad shortage of antivenom now!
Recommended Reading Consuming
This video using data from England (2026-01-14) shows charts for 17 diseases, and makes it clear that infection rates have risen since COVID-19 shows up, and not because of “immunity debt”.
This pair of opinion pieces goes through nine vaccine myths and carefully explains why they are wrong — and how to counter them: Part 1 (2026-01-15) and Part 2 (2026-01-16).
Influenza
Transmission
💨🚫🤧 Well, this is embarrassing. This paper from USA (2026-01-07) put volunteers — infected and uninfected with the flu — into a suite hotel rooms and had them do a bunch of controlled interactions with and without various mitigation measures (e.g. masks, hand washing) to see what activities got the most uninfected people sick. But nobody got sick!
They mentioned that the hotel rooms had “limited ventilation but a high air recirculation rate”. Maybe they did too good of a job of mixing the air, breaking up concentrated plumes of exhaled viruses? Maybe the volunteers already had antibodies to the 2024 strains? Some of them had recently gotten a flu shot, so that was probably part of the problem, but all of it? Maybe the sick participants weren’t sick enough? Difficult to know.
Vaccines
💉 This report from France (2026-01-15) on the effectiveness of the current season’s influenza vaccines reports that the VE against confirmed infection was:
- 36.4% overall;
- 57.2% for children under 18;
- 45.1% for adults between 18 and 64;
- 27.7 for adults over 64.
Measles
Transmission
According to the Government of Canada Measles and Rubella Monitoring Report (updated 2026-01-12), in the week ending 3 January 2025, the following jurisdictions had the following number of measles cases:
- Canada: 32;
- Alberta: 15;
- Manitoba: 9;
- BC: 7;
- Quebec: 1.
