Long COVID
🎉🎉🎉‼️ This case studies paper from USA (2025-02-09) reports that all nine of the study patients who got stellate ganglion blocks for three consecutive weeks improved significantly!
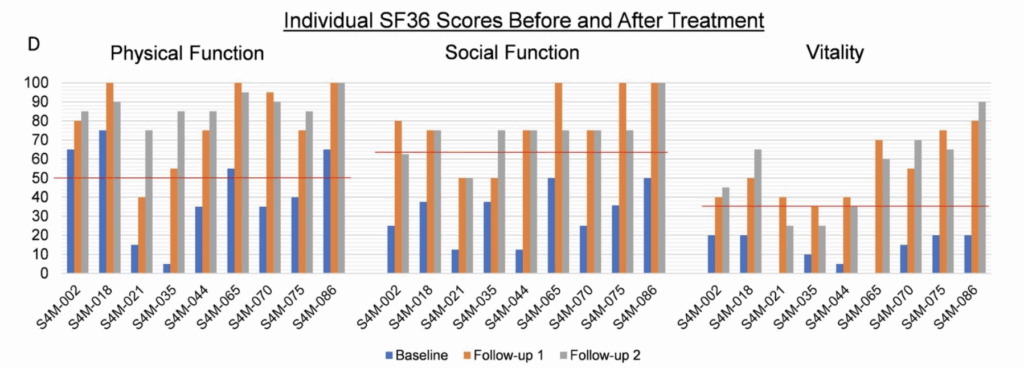
I’m surprised that I missed it in February, and that there hasn’t been more excitement about it, as these are hugely encouraging results!
😢 This study from USA (2025-09-12) and this study from USA (2025-09-16) report that Paxlovid doesn’t reduce the rate of long COVID much, if at all. The second paper did find some age stratification: there was a 7% reduction in people 50-64 y/o, and a 12% reduction in people 65 and older, but almost no effect in people under 50.
In the 2025-09-05 General post, I cited this paper (2025-09-01) which found that people over 70 had significantly lower Long COVID rates than people under 70 — which seems a little strange. I realized that one possibility is that people over 70 get diagnosed less often than they should because it’s harder to distinguish between “Long COVID” and “getting older” with older people than with younger people.
Pathology
This slide deck from the Fall meeting of US CDC’s ACIP meeting (2025-09-19) says that COVID-19 is not, in fact, over. Here’s a breakdown of what respiratory viruses people in the hospital had:
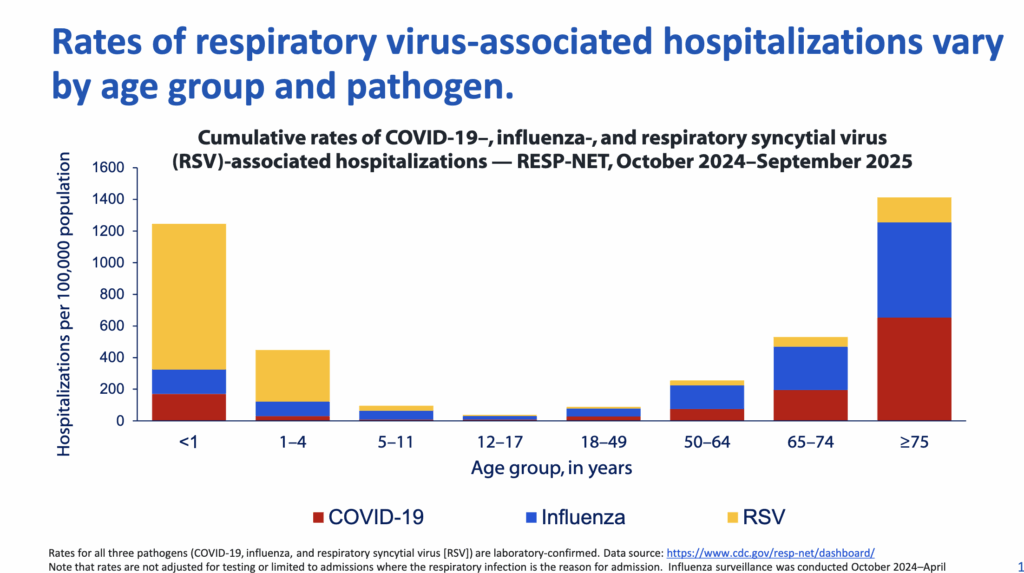
Even in a year which this US CDC report (2025-09-11) says was the worst influenza season in fourteen years, there’s still almost as much COVID-19 as flu in hospitals among people over 50, and a significant amount in infants.
The slide deck also mentioned that 84% of all adults who died in hospital in the USA from COVID-19 were over 50 — but that means that 16% of those who died were under 50. (I couldn’t find death rates for over/under 50 exactly, but this report from the US National Vital Statistics System (2025-09) says that overall, 87.9% of all the people who died in the USA were over 55 and 93.0% were over 45.)
The deck also showed that over the course of the pandemic, the rate of hospitalizations per 100K people was ranked in an almost exactly old/young interleaved manner: oldest, then youngest, then second oldest, then second youngest, then third oldest, then third youngest, then fourth and fifth oldest, then fourth youngest:
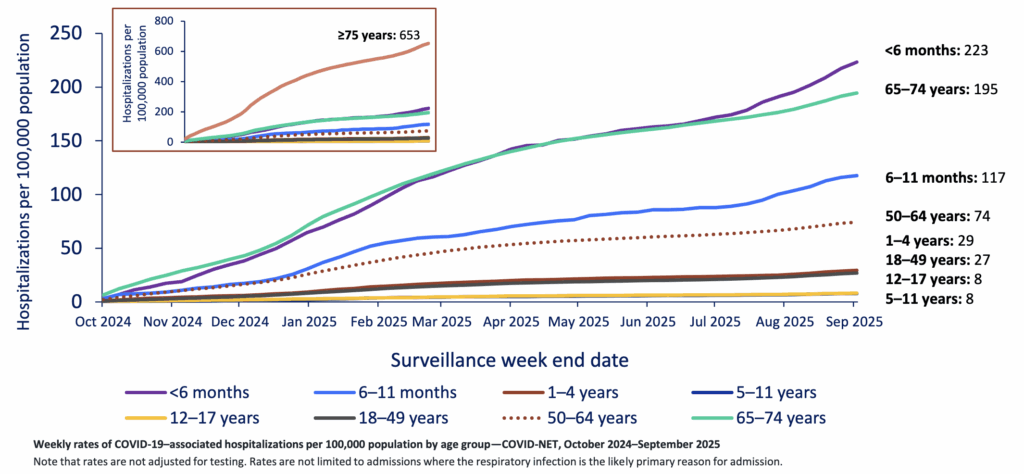
COVID-19 is dangerous for little kids!
🩸 This paper from UK (2025-09-16) reports that Long COVID and menstruation influence each other.
- Women with Long COVID have higher volumes of bleeding, longer duration, and more intermenstrual bleeding than women who never had COVID-19.
- Long COVID symptoms were worse during the perimenstrual (right before and during bleeding) and follicular (immediately after the bleeding) phases.
📆 This paper from USA (2025-08-21) reports that an immunocompromised man had COVID-19 — not Long COVID, but the acute illness — for 750 days. His infection started in mid-May 2020, and mutated over and over again until it looked something like the Omicron variant. While this does not prove that long-lasting infections in immunocompromised people are where big jumps in variant mutations happen, it certainly increases the odds.
While the paper didn’t say anything to this effect, I wonder if the fact that the mutation ended up at Omicron instead of going “past” Omicron means that Omicron is as bad as it’s going to get. I sure hope so!
Testing
😲😲😲💩💧‼️ This thread (2025-09-18) discusses an amazing spike in COVID-19 detections in the wastewater of Coeur d’Alene, Idaho. This graph from this thread (2025-09-18) shows Coeur d’Alene’s wastewater detections compared to every other tested sewershed in the USA:
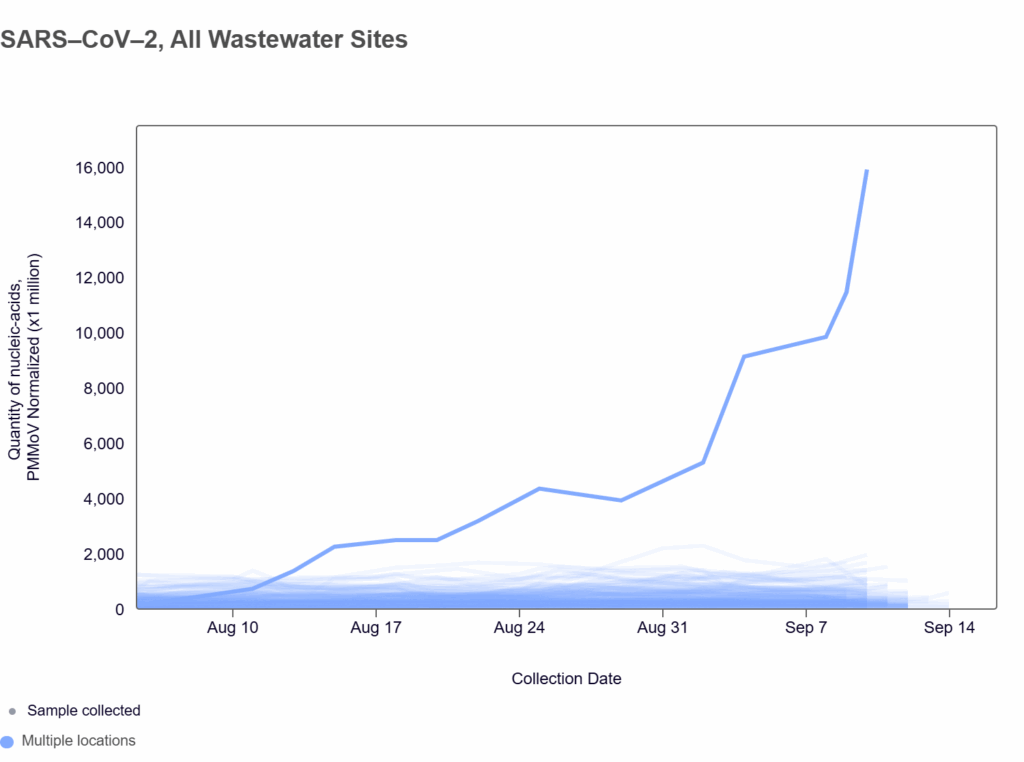
The bulk of the Coeur d’Alene detections are genetically the same, and appears to be a mutant form of BQ.1.1 — which is about 2.5 years old. This makes it highly likely that all this virus it is coming from one person. (This is precedented: there was another case of probably one person shedding a huge amount in Missouri.)
The easy conclusion is that it is another long-lasting infection in someone who is immunocompromised.
Treatments
💊💉 I’ve had people say to me that people will die because Trump’s administration crashing medical research funding and destroying the NIH and CDC will mean better treatments will not get developed. I was more chill about it. I think it’s not quite the right framing to say “people will die” from new drugs not being developed, preferring instead to say that “people will not be saved”. But more than that, I felt that the rest of the world would 💸probably pick up at least some of the slack. After all, the US only has about 4% of the population, surely the other 96% can make breakthroughs as well!
I am willing to admit that going purely by population understates the US’ influence. This article (2021-01-04) says that the US makes up about a quarter of the global economy; I should perhaps say that the other 75% can make breakthroughs.
However, there is a piece I was not paying attention to. This article (2025-09-19) about pharma investments in the UK points out that Trump is telling pharma companies that they have to sell drugs in the US at no higher than they sell for in other countries. Well, the drug companies aren’t willing to discount their US sales, so they are instead raising the prices in other countries and — at least in the UK — cancelling investments. This suggests that the “other 75%” might also see research slowdowns as a result of Trump’s policies. 💸
Mitigation Measures
This paper from USA (2025-09-10) reports on hospital-acquired COVID-19 infections in shared patient rooms.
- 26.3% of people exposed to COVID-19 in hospital developed COVID-19. (The paper doesn’t say if this was from roommates, doctors, or what.)
- Increased measured air changes per hour (ACH) reduced the risk of infection by 12%.
- Room mechanical ventilation (RMV), which they defined as rooms connected to a central HVAC system with “with air supply/exhaust vents or room-level modifications that created RMV” reduced the risk of infection by 49%. (No, I don’t understand what RMV is.)
- Portable HEPA filters did not affect the risk of infection — but they gave no details on the portable filters’ clean air delivery rate, how much of the time they were kept on (did patients turn them off because they were noisy?), where they were placed, etc. One 4″ filter powered by a 3″ fan that was set to LOW 95% of the time wouldn’t be very useful.
Measles
Transmission
According to the Government of Canada Measles and Rubella Monitoring Report (updated 2025-09-15), in the week ending 6 September, the following jurisdictions had the following number of cases:
- Canada: 53;
- Alberta: 22;
- BC: 12;
- Nova Scotia: 8
- Manitoba: 7;
- Ontario: 2;
- Saskatchewan: 2.
