Some weeks, there’s not much news; some weeks there’s a lot. This week had a lot and was a lot for me to process.
Vaccines
💉 CORRECTION! I re-read the PHAC recommendations for who should/may get a second vaccination this year, and I believe that what I said on 2025-08-11 was (probably) wrong. I said that nobody except was in the “may get a second shot” category except people over 80, who live in care homes, and/or are immunocompromised. I now see that the wording is ambiguous, and that people in congregate housing, the clinically vulnerable, pregnant people, health-care workers, racialized minorities, First Nations, and Métis (probably) may get a second shot.
💉 A friend in the USA asked me whether she should get a vax now (in the USA) or wait for the fall strain. Well, it’s complicated.
Circulating Variants
The dominant strain in the US and Canada right now is XFG, with LP.8.1 and NB.1.8.1 declining:
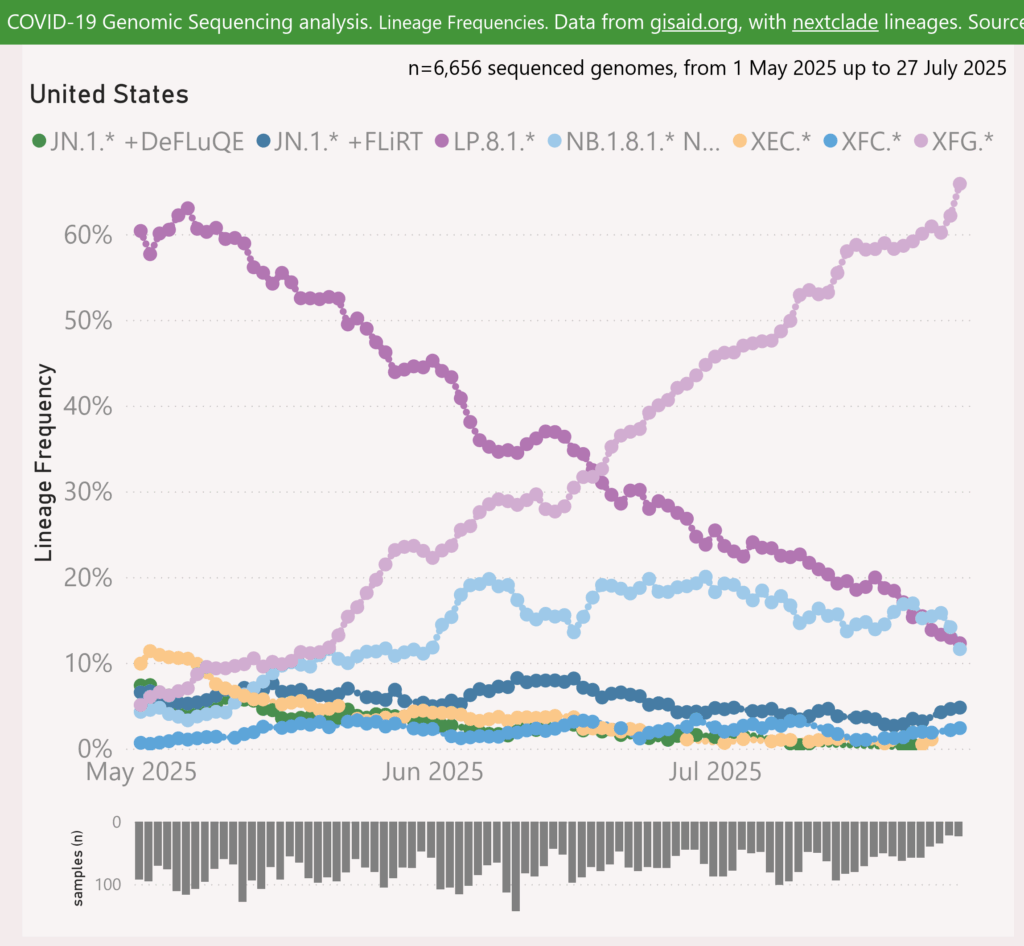
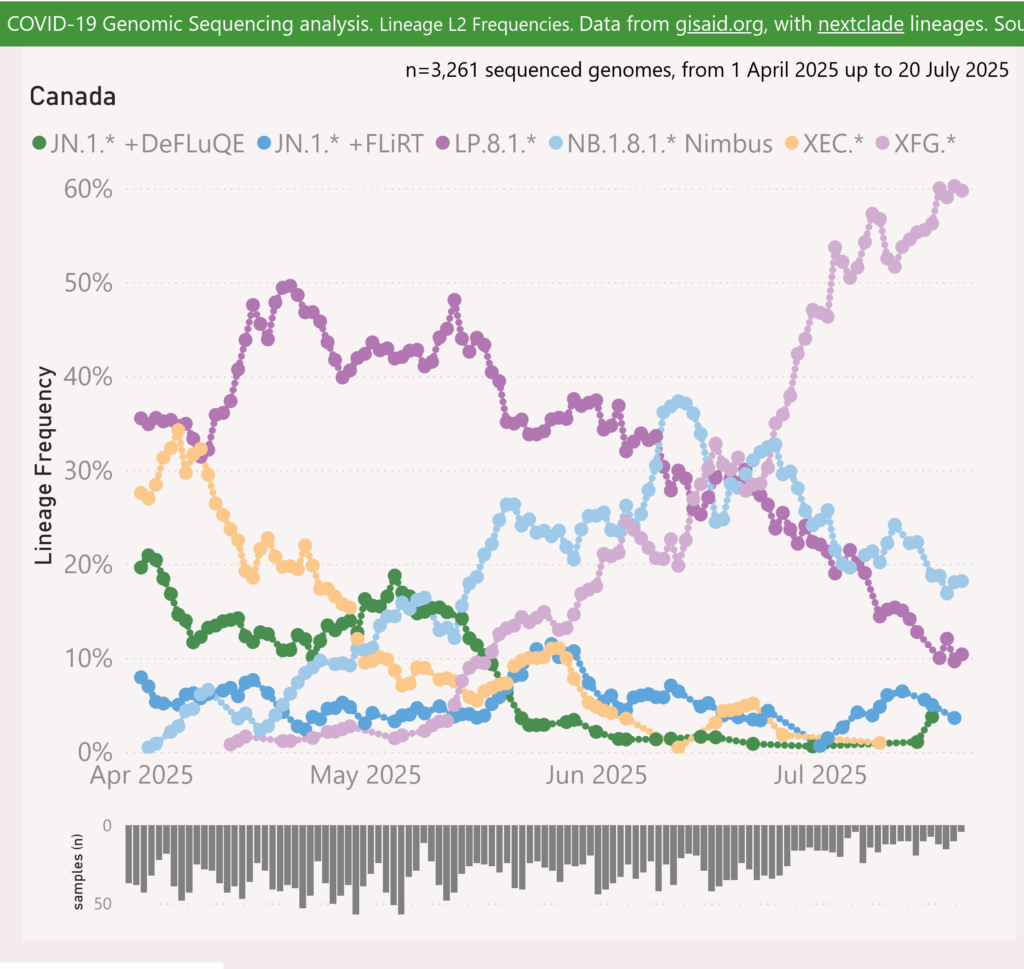
Variant Lineages
This preprint (2025-05-01) says that XFG is a recombination (think “merger”) of the LF.7 and LP.8.1.2 strains.
This paper (2025-01-28) says that LP.8.1 descends from KP.1.1.3, which descends from JN.1., and that LF.7 descends from JN.1.
Let me try to draw a picture:
JN.1 -> KP.1 -> LP.8.1
| +
-----------> LF.7
=
XFG
In other words, XFG is a closer relation to JN.1 than it is to KP.2, and it’s even closer to LP.8.1.
💉 Expected Fall Vaccine Strains (?)
Meanwhile, here’s what I know about what strains will be available.
- 🎉 This press release from Pfizer (2025-08-18) and this release from Moderna (2025-08-22) say that Health Canada just approved their LP.8.1 vaxes for use in people 6 months and up.
- Moderna and Pfizer’s vax from Spring 2025 is based on KP.2 (a child of NJ.1); Novavax is based on JN.1.
- Canada’s announcement (2025-01-10) said that — as far as I can understand — they would use what they used last time, unless something better came along. 🤷
- Canada’s announcement (2025-01-10) says — in my reading of it — that if you are under 65 and don’t have specific risk factors, you may have only one shot per year, so if you got a shot in the Spring, you aren’t getting LP.8.1.
For my readers outside Canada:
- This announcement in a research journal (2025-05-20) says that going forward, the US Food and Drug Administration requires randomized controlled trials for any new COVID vax (including ones based on new strains) that will go into people under 65 without risk factors. I think that means that Pat Average Middle-Aged Person will still be allowed to get a dose of what they got in the Spring, but not any new strain.
- Can Americans come to BC to get COVID-19 vaccine? I talked to a pharmacist, who said no. It’s not that the pharmacies bought the vax and later bill the government for it: the government bought the vax already. The pharmacy has no right to sell it to you, because the vax doesn’t belong to the pharmacy.
- This article (2025-05-22) reports that the US vaccine advisory committee has said that it would prefer manufacturers make LP.8.1-based vax, but are allowed to give JN.1-lineage (which IIUC would include KP.2).
- This article (2025-07-26) says the European Union has done the first stage of approval to Pfizer’s LP.8.1 vax.
Pathology
‼️😬 This paper with data from sixteen countries (2025-08-17) reports that women (but not men) who had COVID-19 now have “older” blood vessels.
Women who had had COVID-19 infections had higher levels of carotid-femoral pulse wave velocity (PWV), a biomarker associated with large artery stiffness — and hence to age. (The amount of stiffening is the same as you’d get from five years of aging. 😬) While the stiffening was a bit worse if you had been in the ICU, there wasn’t any difference between people who had been hospitalized without ICU or not hospitalized at all.
They also found that persistent symptoms in women were associated with higher levels of PWV, regardless of how bad their acute COVID-19 case was and what comorbidities they had.
In other words, COVID-19 ages women’s arteries.
🧬😬 This paper from Iran (2025-08-19) reports that COVID-19 gives you DNA damage, and the worse your COVID-19 case is, the more DNA damage you get:
- patients who were intubated in the ICU: mean of 29.5% of the patient’s DNA (in blood samples) was damaged;
- patients who were admitted to the ICU but not intubated: 24.3%;
- hospitalized patients who did not go to ICU: 19.1%;
- healthy controls: 9.4%.
The authors seemed to really want to tie the DNA damage to Long COVID, but the blood samples for the DNA tests were done only four weeks after the patients’ tested positive for COVID-19. At four weeks, the patients are still recovering from their acute phase!
😬 This paper from Australia (2025-08-16) reports that being on ECMO (heart-lung machine) with COVID-19 is much worse than being on ECMO with H1N1 influenza pre-pandemic. People on ECMO because of COVID-19 were 16.8 times as likely to die as people on ECMO because of the flu. People with COVID-19 also stayed on ECMO for twice as long as flu people.
Long COVID
‼️😬 I don’t usually link to lay articles about research papers because frequently the lay article is overly general, or vague, or gives way more background information than somebody who has some familiarity with the field needs. This article (2025-08-13), however, I feel is a particularly well-written lay summary of this paper from USA (2025-02-05). It reveals things about the paper that I had missed the first time around, when I just read the abstract (in part because I didn’t have access to the full article).
The paper took a novel approach to figuring out just what the incidence of Long COVID is: they did an electronic record search for symptoms of Long COVID, and compared it to an electronic record search for the same terms for pre-pandemic patients and to a search for Long COVID-ish symptoms in people with a negative COVID test. The latter two searches gave them a upper bound for the incidence of these symptoms that were not a result of COVID-19, which then they were able to use to calculate lower bounds on Long COVID:
- for adults, 5 to 6% of people who caught COVID-19 developed Long COVID;
- for children, 1.4% developed Long COVID.
Note that a factor in this being a lower bound is that the electronic records won’t find people who did not seek treatment for their persistent symptoms. (Those people might not have sought treatment for their initial COVID-19 infection either, however.)
‼️ They also showed that — despite vaccines and anti-virals — the rate of Long COVID per infection has not gone down over time (at least for the term of the study period, which included people who got their COVID-19 infections between March 2020 and 31 July 2023). Using the values of the number with/without Long COVID from their paper (unadjusted for the baseline of Long COVID-esque symptoms, which shouldn’t change over time), I got:
| Variant of index infection | number without Long COVID | number with Long COVID | percent of COVID cases turning into Long COVID |
| COVID Classic | 838 617 | 69 580 | 7.7% |
| Alpha | 367 748 | 36 900 | 9.1% |
| Delta | 488 689 | 52 454 | 9.7% |
| Omicron BA.1.1-BA.2 | 823 066 | 87 167 | 9.6% |
| Omicron BA.2.12.1-BA.5 | 646 025 | 94 719 | 12.8% |
| Omicron BQ.1.1-JN.1 | 250 599 | 45 241 | 15.3% |
Or, you can look at their visualization of Long COVID cases per COVID case by variant, split out by which database the data came from (though it’s hard to see):
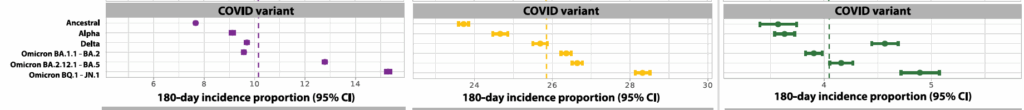
Different colours correspond to different databases that they pulled from. Yellow is data from National Patient-Centered Clinical Research Network (PCORnet). Purple is data from National COVID Cohort Collaborative (N3C). Green is data from PEDSnet, a pediatric learning health system within PCORnet.
They also have a graph of the proportion of COVID-19 cases which become Long COVID cases over time.
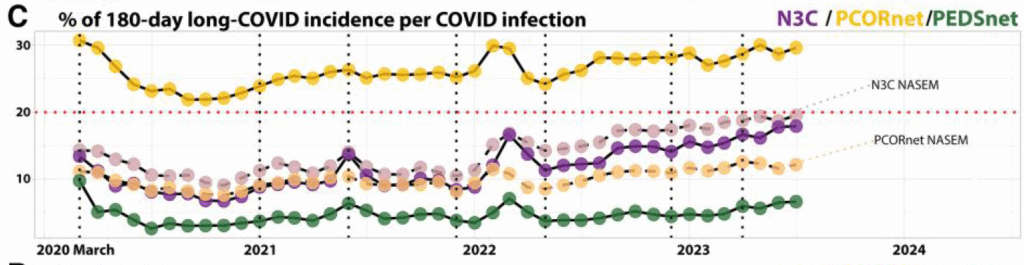
Different colours correspond to different databases that they pulled from. Yellow is data from National Patient-Centered Clinical Research Network (PCORnet). Purple is data from National COVID Cohort Collaborative (N3C). Green is data from PEDSnet, a pediatric learning health system within PCORnet. Pink is data from N3C but using the National Academies of Sciences, Engineering, and Medicine (NASEM) definition of Long COVID. Light yellow is data from PCORnet but using the NASEM definition. Addendum 2025-09-22 I asked one of the authors what the vertical lines were. The first five are different variants (COVID Classic, Alpha, Delta, BA.1.1–BA.2, BA.2.12.1– BA.5, and BQ.1.1–JN.1); the last line is the line after which patients only get a six-month followup, not a one-year followup..)
I don’t know what the dashed vertical lines on the graph are. I thought it might be for the start of different waves, but there’s one more dashed line than wave. I don’t know why there are some bumps (for all the databases in 2022, and for two of them in 2021).
‼️😬 It looks like the rate of Long COVID per COVID-19 infection is rising! Note that, as far as I can tell, “index infection” is “most recent infection before they developed Long COVID”, so that if a patient had an Alpha infection and a Delta infection and an Omicron BQ.1.1 infection, for the table above, they’d only be counted as as a BQ.1.1 infection.
You, like me, might look at the numbers and say that 15% is way higher than what you see from your friends in the real world. Remember that:
- this only includes people who sought medical attention for COVID-19 or Long COVID — people who didn’t seek attention for either won’t show up in the database;
- your friends might not talk about it;
- your friends might think it’s due to something else;
- not all Long COVID is crushing fatigue that leaves you bedbound — it also includes muscle pain, headaches, fatigue, brain fog, loss of smell/taste, and a whole lot of other mysterious things that you could ascribe to e.g. “getting older”.
This paper also found that the older an adult was, they more likely to they were to develop Long COVID. For children, it was reversed: younger children were more likely to develop Long COVID than older children.
Other things they found were risk factors for Long COVID are the same as many other studies: being female, having pre-existing conditions, and having more severe COVID-19 illness.
‼️😬 This preprint from USA (2025-08-13) reports that people who had a COVID-19 re-infection were 35% more likely to get Long COVID than people who did not get reinfected.
The study cohorts are a little tricky to explain: they made sets of matched pairs out of people who had all had at least one infection. When one of the pair caught COVID-19, then that person was assigned to the non-control cohort and the other person of the matched pair was assigned to the controls. So the non-controls all had exactly one more infection than the their paired counterpart, but they all had at least one infection.
They also found that when you got your vaccination mattered. If we call the most recent infection (i.e. the one that got you put into the non-control cohort) “most recent” and the one before that “prior”, the reinfected had the following higher risks of Long COVID than their matched controls:
| vaccinated before prior | vaccinated before most recent | increased risk of Long COVID |
| Yes | Yes | +21% |
| No | Yes | +19% |
| Yes | No | +45% |
| No | No | +33% |
In other words, you always had a higher risk of Long COVID after a reinfection than if you hadn’t gotten reinfected, but the more recently you got a vaccination, the lower your risk of Long COVID. (NB: This might be a purely temporal effect, but it might also be an effect of the newer vax being a closer match to the strain of the most recent infection.)
😬 This preprint from Brazil (2025-07-29) reports that in a cohort of people between 60 and 80, those that had had COVID-19 infections had worse inhibitory control, cognitive flexibility, and working memory than people who had not had COVID-19. Being married and engaging in cognitively-stimulating activities before the infection reduced the degradation in executive function somewhat.
🎉 This paper from USA (2025-07-29) reports that Long COVID patients who did several kinds of fasting / no-sugar diets improved significantly. Before you run off and do heavy fasting, please go watch Gez Medinger’s videos (like this one) on fasting as a Long COVID treatment. He says that fasting helped him a lot, but that it’s really really really hard and says you really shouldn’t do it without supervision.
COVID-Related Excess Death and Sickness
🦀😬 This paper from Taiwan (2025-08-14) reports that people who had had COVID-19 had higher risks of HPV-related cancers than people who never had COVID-19 — by a lot. Compared to matched healthy controls, the COVID-19 cohort had:
- cervical cancer: +67% higher risk;
- vaginal cancer: +131%;
- vulvar cancer: +98%;
- anal cancer: +92%;
- oropharyngeal cancer: +78%.
🩸 This paper from USA (2025-08-06) reports that people who had been hospitalized for COVID-19 infections were:
- 42% more likely to develop high blood pressure than people who had had COVID-19 infections but had not been hospitalized;
- 57% more likely to develop high blood pressure than people who hadn’t had COVID-19 infections.
Non-hospitalized COVID-19 patients weren’t statistically significantly more likely to develop high blood pressure than people who never had a COVID-19 infection.
😬 This paper from Portugal (2025-07-31) reports that among a cohort of people who had been hospitalized for COVID-19, a lot of them had mental health issues afterwards, although they improved over time. The percent of people who had various conditions at three and six months was:
| condition | at 3 months | six months |
| anxiety | 22.2% | 12.0% |
| depression | 23.1% | 11.1% |
| PTSD | 7.7% | 2.6% |
Some subgroups had higher risks for specific conditions:
| condition | characteristic | increased risk |
| anxiety | female | 4.86 times |
| anxiety | elevated ferratin levels | 8.25 times |
| depression | trouble breathing | 1.62 times |
| depression | psychiatric history | 3.44 times |
| anything | anything else they looked at | no increased risk |
‼️☠️😬 This preprint using data from UK (2025-08-02) reports that all-cause mortality is higher in people who had one COVID-19 infection between 31 Jan 2020 to 19 Dec 2022 than controls who did not. Compared to controls, people who had one COVID-19 infection:
- had a +139% higher risk of dying from any cause (+529% ‼️ for those hospitalized and +23% for those who were not hospitalized);
- +45% risk of dying from circulatory issues;
- +98% risk of dying from digestive issues;
- +154% risk of dying from genitourinary issues;
- +120% risk of dying from neurological issues;
- +39% risk of dying from respiratory issues;
- +242% risk of dying from “external causes” (mostly accidental injury);
- +53% risk of dying from cancer.
‼️😬 This paper from USA (2025-08-13) reports that people who had been hospitalized for COVID-19 had a much higher risk new diagnosis with various pulmonary conditions than people who had not had COVID-19:
- pulmonary fibrosis: ‼️ 71.33 times;
- pulmonary hypertension: 16.25 times;
- emphysema: 15.45 times;
- unspecified COPD: 9.28 times;
- chronic bronchitis: 8.95 times;
- subsequent pneumonia: 8.14 times;
- pulmonary embolism: 7.36 times;
- overall: 3.36 times.
😬 This older paper (2022-03-09) from Belgium reports that, among people over fifty, those who were diagnosed with a COVID-19 infection had a 15% higher risk of shingles than those who did not have COVID-19 infections. People over fifty who were hospitalized with COVID-19 had a 21% higher risk of shingles than people over fifty who never had COVID-19.
😷😬 This article (2025-08-17) about this paper which uses data from USA (2025-06-25?) reports that people who had COVID-19 have higher risks of inflammatory diseases of the airway compared to healthy controls:
- asthma: +65.6% higher risk;
- allergic rhinitis: +27.2%;
- chronic rhinosinusitis: +74.4%.
COVID-19 vaccination reduced the risk of asthma by 32.2%, with significant but smaller reductions for allergic rhinitis and chronic rhinosinusitis.
Testing
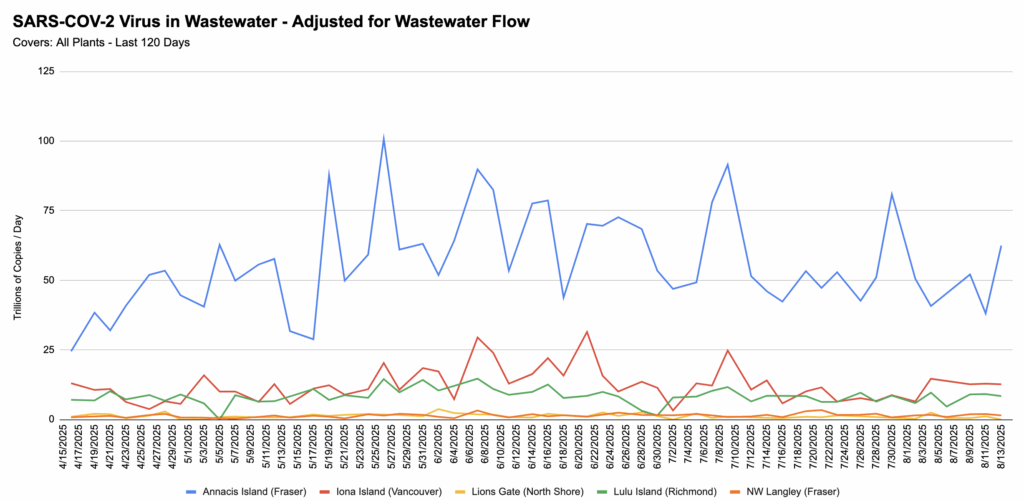
BC Wastewater
💩💧 From Jeff’s wastewater spreadsheet:
Mental Health
😬 This paper from USA (2025-08-12) looked at differences in California adolescents between pre-pandemic (November 2016 to November 2019) and after the mitigation measures were mostly abandoned there (October 2020 to March 2022). They found that adolescents had lower cortisol production, higher levels of systemic inflammation, and reduced prefrontal cortex neural activity. They noted that these effects look a lot like Early Life Stress (ELS), which has demonstrated long-term health effects.
A beef I have with this study is that they repeatedly talk in terms of the measurements being “post-lockdown”, as if everything was hunky-dory during October 2020 to March 2022. I would like to suggest that things were not hunky-dory during this period! The astonishing effectiveness of the mRNA drugs wasn’t announced until November 2020, and the rollout wouldn’t have gotten to most teens until probably late 2021. These teens were living under the cloud of a disease that could kill them; no wonder they were stressed!
Recommended Reading
This blog post (2025-08-18) goes into some depth about the highly negative impact of COVID-19 on blood vessel health.
This article (2025-08-19) explains why the “immunity debt” theory — the theory that the isolation of lockdown suppressed “normal” infections, making our immune systems lazy — is bullshit. It explains that “immunity reset” — damage to the immune system from SARS-CoV-2 — is more likely.
This article (2025-08-13) tears apart a report that RFK Jr. released to justify yanking half a billion dollars in grants for mRNA vaccine research. The report cites research which absolutely does not say that mRNA vaccines are dangerous.
One thing that the report says is that the the spike mRNA is inherently dangerous, so we shouldn’t be giving it to people. I agree that the spike protein is dangerous — especially if you inject it straight into the bloodstream instead of into the muscle (which drains into the lymphatic system, which is not supposed to connect to the bloodstream). However, you don’t get a choice about getting SARS-CoV-2’s spike protein. Either you get a controlled amount from a vaccination, or you get an uncontrolled amount from an infection. (I suppose you could also work really hard to not catch COVID-19 and not get a vaccination, but very few people are willing to work hard to not catch COVID-19 (by masking at all times, purifying their indoor air, etc.), and all the people I know (including myself) who do take strict mitigation measures also get vaccinated every chance they can get.)
Measles
Transmission
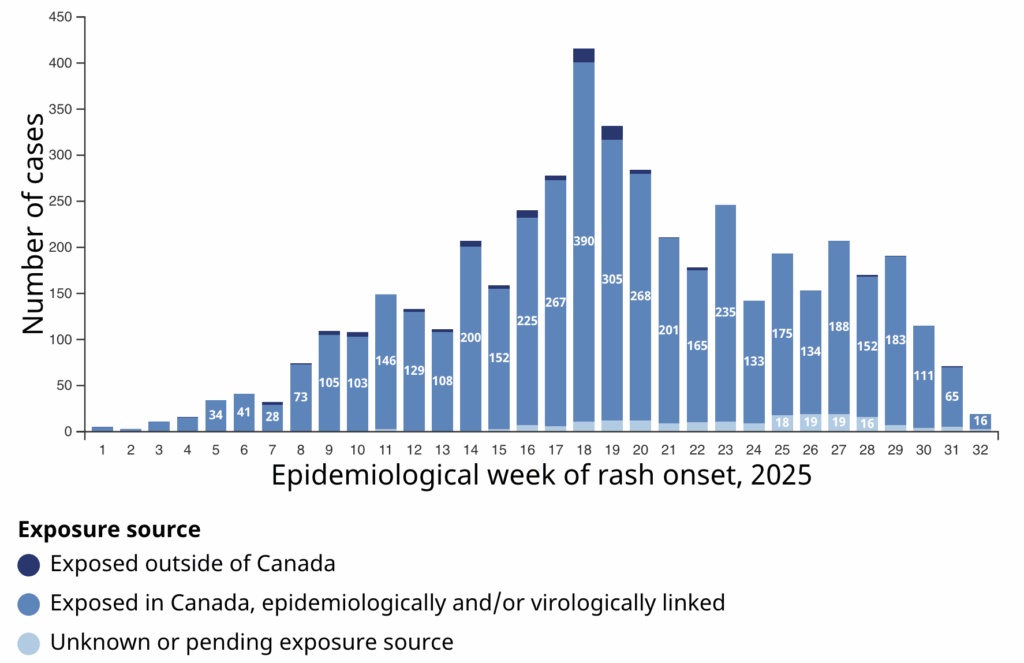
According to the Government of Canada Measles and Rubella Monitoring Report (updated 2025-08-05), in the week ending 26 July, the following jurisdictions had the following number of cases:
- Canada: 94;
- Alberta: 65;
- BC: 18;
- Ontario: 5;
- Manitoba: 4;
- Saskatchewan: 2.
This is down from previous weeks, yay! Don’t look at the last week in this graph — there might be more cases yet to come — but Week 30 and Week 31 probably have all their data in, and they show declining numbers as well, yay!