Mitigation Measures
This paper from eastern Massachusetts found that school districts which dropped mask mandates right away had 44 cases of COVID-19 per 1000 students/staff (accounting for 30% of cases) compared to schools which kept masks. (Before they were allowed to drop mask mandates, the case rates were similar.) Here’s a Twitter thread with an explainer.
Long COVID
This preprint from the USA found multi-factor biomarkers which were good predictors of Long COVID, with low cortisol (a stress hormone) levels being the most predictive marker. (This Twitter thread has a nice explainer.) One thing I thought was interesting is that Long COVID patients had higher levels of antibodies to the herpesviruses Epstein-Barr Virus (EPV) and chickenpox than controls. (EBV has been implicated in all kinds of nasty diseases, including Multiple Sclerosis, and this paper also found higher levels of EBV in long haulers than controls.) They also did not find elevated levels of auto-antibodies, except in a subgroup which had tinnitus and nausea.
This article talks about drug trials for treating Long COVID. There are 26 trials currently underway, but clearly there could be more. The article also gives some reasons for why there aren’t more trials:
- The science is poorly-understood. Trials are expensive enough that researchers are not inclined to just throw drugs at the wall and see what sticks: they need to feel pretty sure it will work, and to do that they need to be able to convince themselves why it should work.
- The drugs they need for the studies are often expensive and in short supply.
- For those scientists considering trials, they are reeeeally leery of saying so, because Long COVID patients are so desperate that they’ll try anything. The researchers want to be pretty certain that something will help before launching a stampede of people to try that treatment.
A report from the US using Census Bureau data found that 35% of people who self-reported as having COVID-19 self-reported as having symptoms for more than three months.
Using general Census data, they find a change in the slope of people who have difficulty with various things, especially difficulty remembering, especially among those without college degrees:


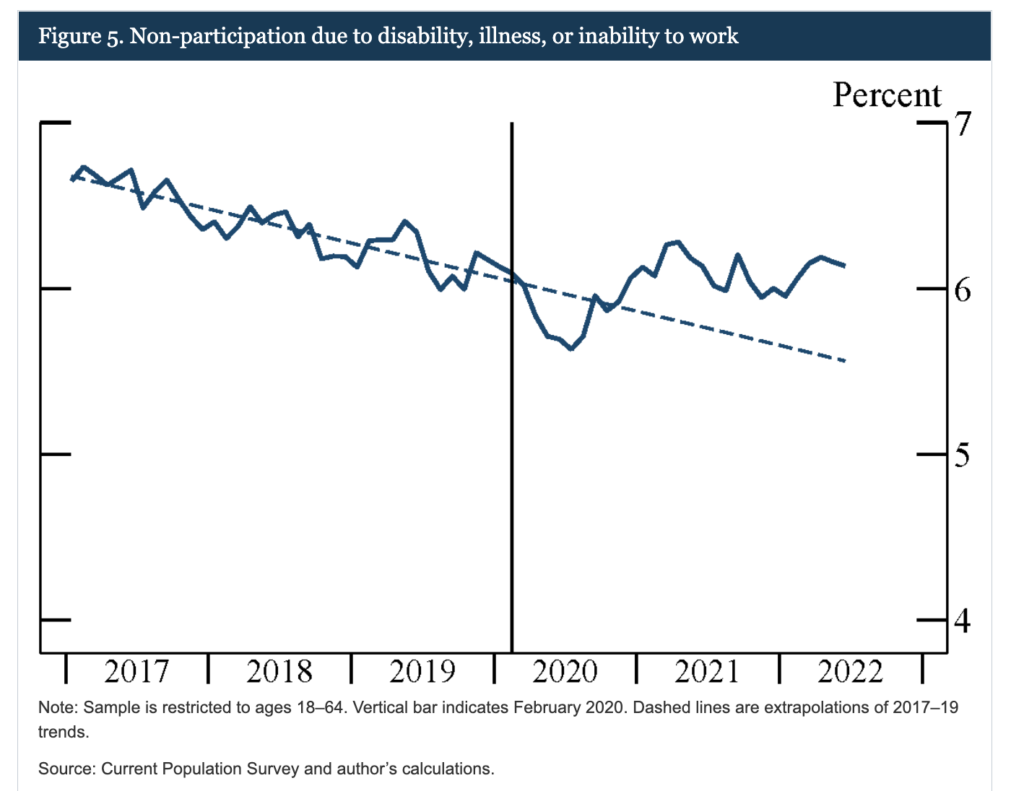
They also found that the percentage of people out of the workforce due to disability was 0.6% higher than expected:
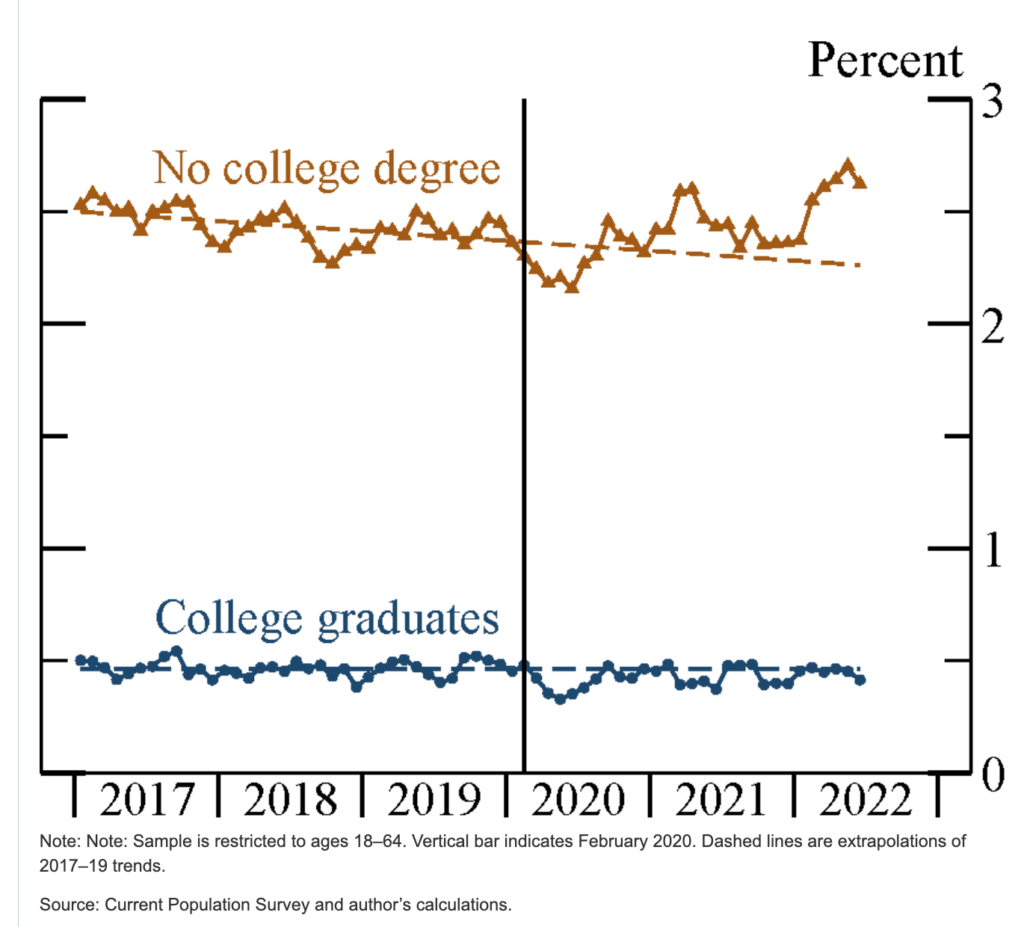
and the college/no-college split was even starker than for cognitive difficulties:
This study from Netherlands found that 12.7% of COVID-19 patients had Long COVID symptoms three to five months after infection.
The research paper doesn’t appear to be available yet, but this article says that researchers have found that Long COVID and ME/CFS patients both have trouble processing calcium, and that calcium levels in cells are too low.
Testing
This article reports that Health Canada has approved a saliva-based PCR-quality COVID-19 test. (Yay, no more swabs!)
Treatments
This paper from the USA says that vaccinated macaques make better antibodies than humans. (!) More specifically, they make antibodies which target a different, more “conserved” (i.e. which doesn’t change as much from variant to variant) part of the spike protein. The antibodies even were as effective against the original SARS, SARS-CoV-1!
The authors talked about how this could be used to make better vaccines, but I didn’t understand how. The authors did not talk about making new monoclonal antibody treatments, though it seemed to me that would be the obvious next step. I’m not a biologist, sue me.
This preprint from the USA and Austria says that some single-point virus mutations would make Paxlovid much less useful, and calls for developing a cocktail. This preprint from the USA and China says the same thing.
This preprint says that the risk of having a COVID-19 rebound after treatment with Paxlovid rebound is 32% higher for BA.5 than for BA.2.12.1.
This preprint says that rebound is more likely in patients who have gotten Paxlovid than in those who did not get Paxlovid.
Pathology
SARS-CoV-2 infects the brain; that is known. But how? There are no ACE2 receptors in the neural tissue that SARS-CoV-2 infects. This paper says that SARS-CoV-2 gets in via the NRP1 receptor.
I am still not a biologist, but this feels like a BFD to me. Knowing which receptor SARS-CoV-2 is getting in via means we have a hope of jamming it up.
Recommended Reading
If you like nerding out about new vaccines like I do, this blog post gives a list of all THIRTY-THREE of the vaccines which have finished Phase 3 (yay!).
